Step By Step Guide For Accidental Needle Sticks in Healthcare: Expert Solutions From Secure Waste
Have you ever found yourself in a situation where you accidentally punctured your skin with a sharp needle or other healthcare sharps, such as a scalpel?
The experience can be alarming, but it is crucial to remain calm and informed. Secure Waste offers expert guidance and comprehensive solutions to help you navigate this potentially hazardous scenario.
The risks associated with being punctured by a sharp object are significant, underscoring the importance of being well-prepared and familiar with the necessary steps to take in such an event. Knowing how to respond quickly and effectively can make all the difference in ensuring your safety and well-being.
6 Things You Should Never Do With Sharps Needles” Secure Waste Explains In A Step By Step Guide

I Just Got Stuck With A Sharps, Now What?
Needlestick injuries are not just minor accidents; they are serious incidents that require immediate attention and should never be taken lightly. Such injuries significantly increase the risk of exposure to various dangerous and highly infectious pathogens, making it essential for individuals to be well-informed about the correct actions to take in the unfortunate event of a needlestick injury.
Even under the most vigilant circumstances and despite healthcare professionals’ best efforts to prevent them, needlestick injuries can still occur, often with alarming frequency. Statistics from the Centers for Disease Control and Prevention (CDC) highlight that disposable syringes and suture needles are the predominant devices associated with these sharps-related injuries.
The urgency of this issue was magnified during the height of the COVID-19 pandemic, when studies indicated a disturbing rise in needlestick injuries. This surge is likely attributed to the heightened strain and fatigue experienced by healthcare workers as they navigated the intense pressures of the pandemic. Therefore, healthcare professionals must know what steps to take should they suffer a needlestick injury.
Need Local Sharps Needle Disposal? Contact Secure Waste For Expert Sharps Solutions!
Increased awareness diminishes the occurrence of needlestick injuries.
Accidents can happen in any environment, but one of the most effective strategies to prevent needlestick injuries in healthcare settings is through comprehensive training and a heightened sense of awareness. Research has shown that safety protocols significantly improve when healthcare workers receive thorough education about handling and disposing of sharps. The study found a marked reduction in overfilled and improperly disposed sharps containers when targeted training programs and informative educational posters were introduced.
Despite these strides toward improvement, it is alarming to note that over 300,000 healthcare professionals fall victim to needlestick or sharps-related injuries each year. All healthcare workers must know the risks and the essential steps to take immediately following an injury. This knowledge is vital for their safety and the well-being of their patients.
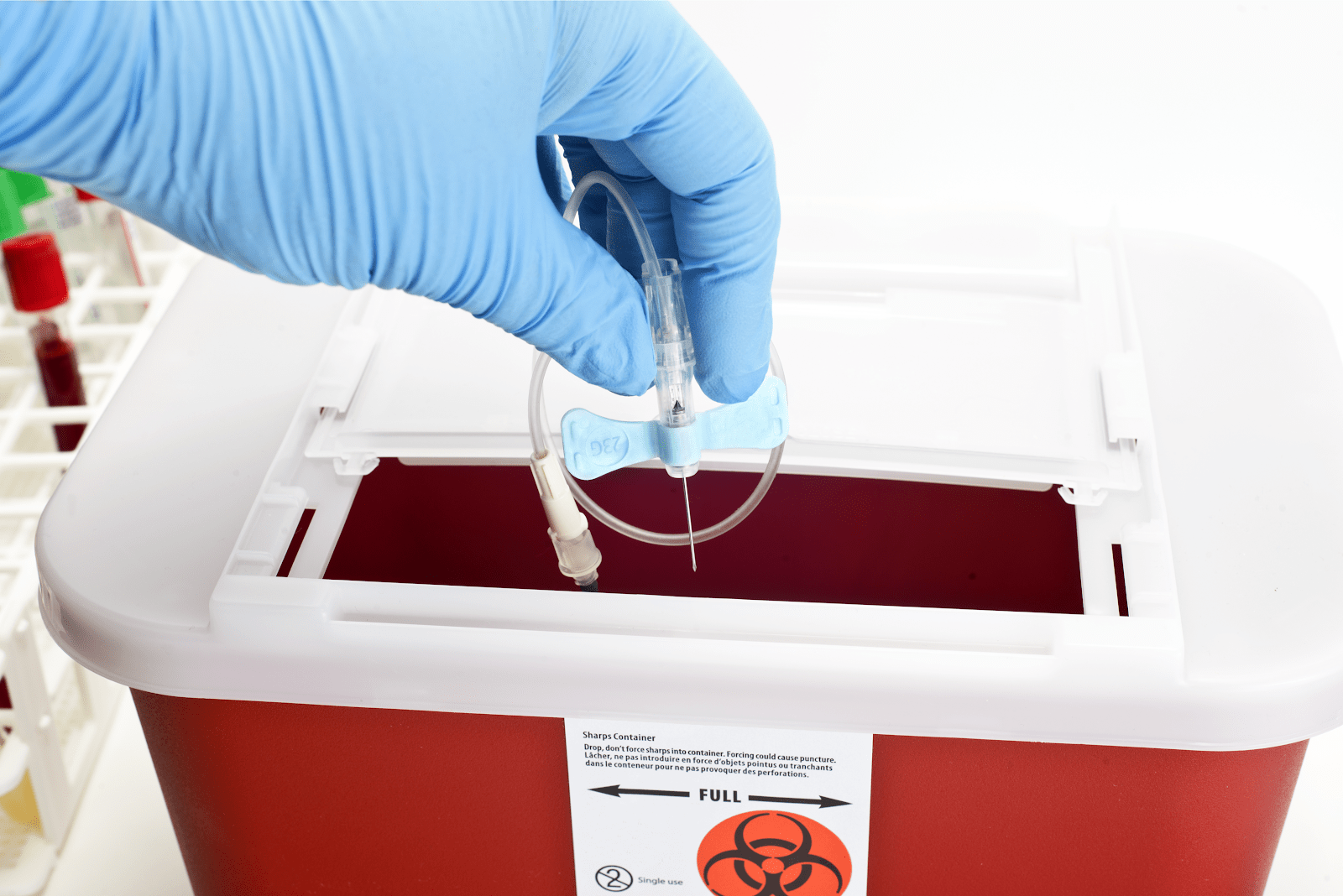
Actions to take right away following a needlestick injury
According to the National Institute for Occupational Safety and Health (NIOSH), acting swiftly following a needlestick injury or potential exposure to a patient’s blood or body fluids is crucial. The specific steps to be taken hinge on the type and context of the exposure:
- Immediate Care: Begin by thoroughly washing the needlestick site with soap and water to cleanse the area and minimize the risk of infection. Additionally, suppose there is exposure to the eyes. In that case, irrigating them vigorously with saline or clean water is essential, ensuring the flush is thorough to remove any harmful contaminants.
- Surface Decontamination: To further reduce potential harm, exposed areas such as the nose, mouth, or unprotected skin should be flushed with water.
- Incident Reporting: After addressing immediate medical needs, reporting the incident to supervisors as soon as possible is essential. Some healthcare professionals may feel inclined to postpone this crucial step due to a busy schedule or may downplay the seriousness of the situation out of embarrassment or fear. Nonetheless, it is vital to prioritize seeking medical guidance and treatment for possible exposures to serious infections such as HIV, hepatitis B, hepatitis C, or others. Post-exposure prophylaxis and management are critical interventions safeguarding healthcare workers’ health and protecting patients and colleagues from exposure.
- Facility Protocols: Familiarity with and adherence to facility procedures for reporting exposures are essential. However, do not hesitate to pursue testing or to initiate prophylactic treatment in the meantime.
- Vaccination Recommendations: In situations with potential exposure to hepatitis B or C, the affected healthcare professional should undergo testing and may need vaccination. While vaccination may not always be mandated, it is strongly encouraged. Individuals are also recommended to complete post-vaccination testing to ensure immunity.
- Timely Testing: Healthcare personnel must undergo testing within 48 hours of a potential exposure to hepatitis C (HCV). Follow-up testing should be performed three and six weeks after the exposure to monitor changes.
- Addressing HIV Exposure: If there is a potential exposure to HIV, initiating post-exposure prophylaxis with antiretroviral drugs is highly recommended. This intervention should commence within 72 hours of the incident to effectively halt the possibility of seroconversion.
- Ongoing Support and Follow-Up: Further appointments and follow-up processes may involve up to six months of continued testing, monitoring for drug toxicity, and counseling support. This counseling can be highly beneficial, assisting the injured individual in navigating the emotional challenges of stress, fear, and uncertainty often accompanying such exposures.
These steps are not merely procedural; they represent a vital commitment to protecting the well-being of healthcare professionals and their patients.

Recording a needlestick injury with OSHA
Documenting needlestick injuries is crucial for employees’ health and safety and ensuring compliance with the regulations set forth by the Occupational Safety and Health Administration (OSHA).
Specifically, needlestick injuries are covered by Standard 1904.8, which outlines the record-keeping requirements for injuries caused by needlesticks and sharp objects.
According to OSHA’s guidelines, it is essential to record all work-related needlestick injuries and cuts from sharp objects contaminated with another individual’s blood or other potentially infectious materials (as defined in 29 CFR 1910.1030). These cases must be documented under the injury category on the OSHA 300 log.
To maintain the confidentiality of the affected employee, the log must not include the employee’s name, as required by privacy case requirements specified in paragraphs 1904.29(b)(6) and 31904.29(b)(9).
This documentation requirement applies only to work-related incidents that involve contamination from blood or other potentially infectious materials (OPIM).
Furthermore, should an employee later receive a diagnosis of an infectious bloodborne disease linked to a documented needlestick injury, the OSHA 300 log must be updated.
This update must reflect the correct classification of the case, particularly in situations of job transfer, restricted work duties, days away from work, or the unfortunate event of the employee’s death.
The log must include a detailed description of the infectious disease and update the classification from an injury to an illness, ensuring accurate and comprehensive record-keeping as mandated by OSHA.
What Is the OSHA Form 300 Log? Example Below
This comprehensive log book is designed specifically for healthcare facilities to meticulously record occurrences of accidental sharp needle stick injuries The OSHA 300 Log Book is essential for ensuring workplace safety and compliance with Occupational Safety and Health Administration OSHA regulations It captures crucial details such as the date and time of each incident the type of sharps involved the circumstances surrounding the injury and subsequent actions taken By maintaining accurate and detailed records healthcare organizations can analyze trends implement preventive measures and enhance training programs to protect healthcare workers from these potentially hazardous exposures
In conclusion-
Now that you have a more comprehensive understanding of accidental needle sticks and how to manage them, don’t hesitate to contact Secure Waste.
We provide reliable, compliant, eco-friendly medical waste disposal solutions for your facility’s needs. We have expertise in biomedical, hazardous waste, and Sharps container disposal. In addition, we provide customized waste management plans, including secure collection and transport, and sustainable disposal practices.
Contact us today for a FREE Waste Assessment, or request a quote online!

Expert Medical Waste Management: With over 25 years of industry experience, Secure Waste is a trusted local leader in hazardous and biohazardous waste disposal across Maryland, Virginia, and Washington, D.C. Specializing in medical waste management, sharps needle disposal, and biohazard waste removal, the company ensures full compliance with federal, state, and local regulations while prioritizing environmental sustainability.
The company also offers additional services, including secure document shredding and sharps container sales, providing comprehensive solutions for healthcare facilities and businesses. Our cost-effective services help clients maintain regulatory compliance without unexpected costs.
With a commitment to customer satisfaction, Secure Waste offers tailored waste management plans that align with industry best practices. Their team of experts provides reliable, timely, and compliant services, making them the preferred choice for medical waste disposal. For a free waste quote or more information, visit www.securewaste.net






