The Rising Cost of Hospital Waste Management and How to Control It
Introduction
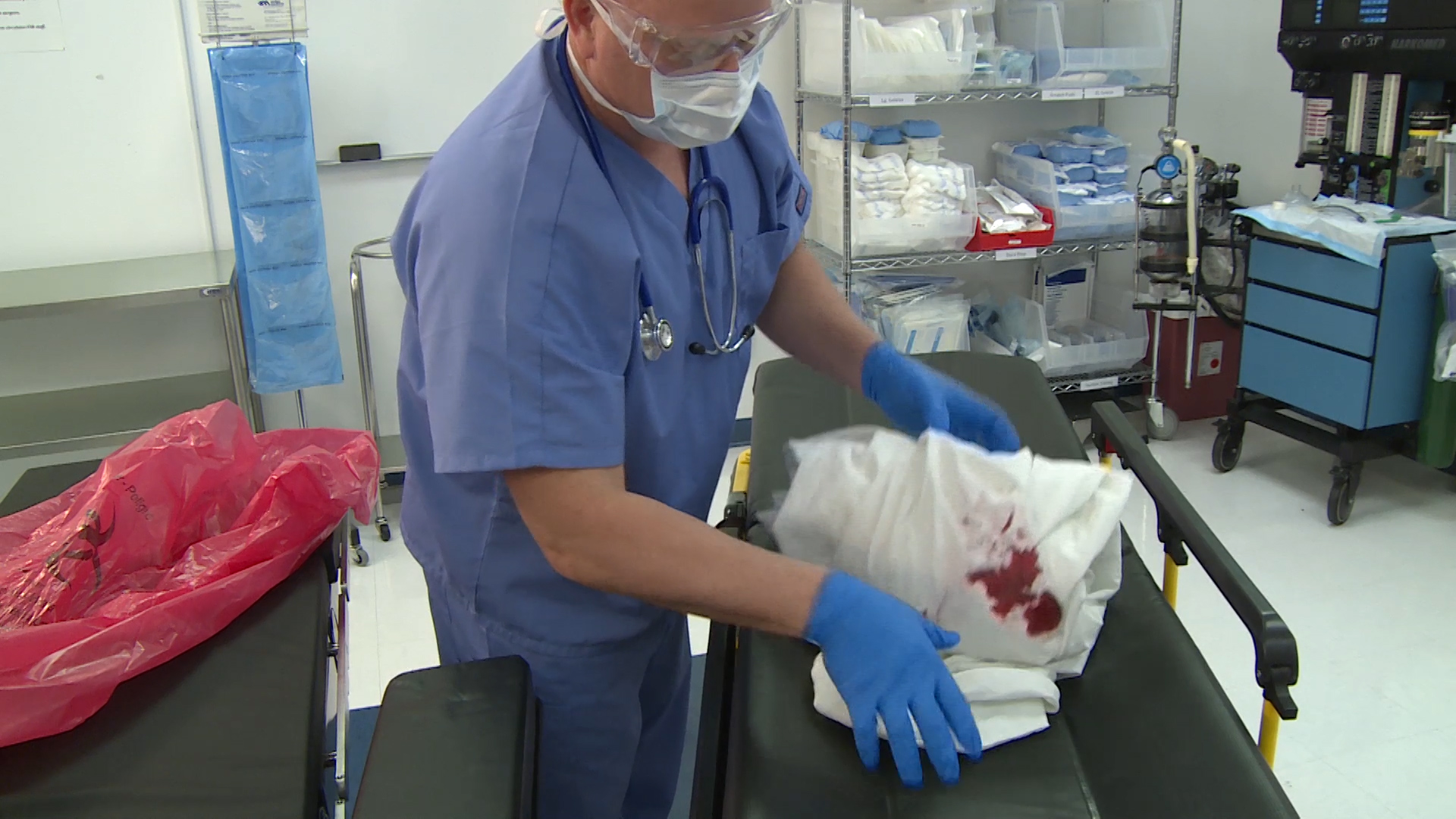
Hospital waste management is becoming an increasingly expensive challenge for healthcare facilities worldwide. The volume of waste generated by hospitals is growing from used gloves and syringes to discarded medical supplies and even human tissue. In the United States alone, hospitals produce roughly 7,000 tons of garbage daily at a total annual disposal cost of around $10 billion.
Improper or inefficient waste handling practices add even more to the bill – American medical facilities are estimated to overpay about $7 billion yearly on waste management due to suboptimal practices like overusing single-use items and poor segregation of medical waste. These rising costs aren’t just line items on a budget; they translate to money that could otherwise be spent on patient care, staff, or new medical technology.
Why are waste disposal costs for hospitals so high and climbing higher? Part of the answer lies in the strict requirements for handling regulated medical waste (RMW) – the biohazardous or infectious waste that must be specially treated. Disposing of RMW is significantly more expensive than disposing of ordinary trash.
Treating and disposing of medical waste can cost 7 to 10 times more than typical solid waste disposal. Ideally, only a small fraction of a hospital’s trash (around 10% or less, even as low as 3-5% per CDC guidelines) should be RMW. However, many hospitals struggle with waste segregation, and studies find that RMW constitutes 20-40% of total waste in facilities with poor disposal practices. The outcome is predictable: hospital waste bills skyrocket as tons of what could have been ordinary trash or recyclable material end up in red biohazard bags destined for high-cost treatment.
The financial impact of mismanaged hospital waste goes beyond just disposal fees. Hospitals incur hidden costs from regulatory fines, inefficiencies, and lost resources when waste isn’t handled correctly. This article explores the factors driving up waste management expenses in healthcare, the often unseen costs of poor waste practices, and — most importantly — what hospitals can do to rein in these expenses.
By implementing better waste segregation, innovative procurement, staff education, and sustainable practices, healthcare facilities can significantly cut waste-related costs (by as much as 40-70% in many cases) while improving safety and environmental outcomes. Let’s examine the causes and solutions for the rising cost of hospital waste management.
Why Hospital Waste Disposal Costs Are Rising
Several converging factors have increased hospital waste disposal costs in recent years. Understanding these drivers is the first step toward controlling expenses:
- Over-Classification of Waste as “Biohazardous”: A primary cost driver is the misclassification of general waste as regulated medical waste (RMW). When staff toss non-infectious trash (packaging, paper, food waste, etc.) into red biohazard bags, the hospital pays a premium for disposal.Special medical waste treatment (incineration, autoclaving, etc.) costs about 10 times more than landfilling regular solid waste. In some hospitals, poor segregation practices have caused RMW to make up 20–40% of total waste (far above the ~10% target). This means the facility is paying hazardous waste rates to dispose of what is often ordinary trash. One analysis warned that placing RMW bins in public or patient areas invites misuse – mixing regular garbage into biohazard bins can reduce disposal costs by more than 70% for that waste. In short, every pound of waste unnecessarily treated as “medical” waste is an avoidable expense.
- Reliance on Single-Use Supplies and Materials: Modern hospitals use many disposable items for infection control and convenience – from surgical instruments and gowns to one-use device kits. This “throw-away” culture leads to larger waste volumes and higher disposal bills.Supply chain expenses account for about one-third of a hospital’s operating budget, which is a waste. For example, studies found theaverage operating room disposes of $968 worth of unused medical supplies per surgery (nearly $3 million in wasted supplies per OR annually).Those unused items go straight into the trash, representing a loss of the item’s purchase cost and added cost to treat or haul it away. The healthcare industry’s heavy use of single-use plastics (tubing, packaging, syringes, etc.) compounds the waste problem.
During the COVID-19 pandemic, this issue intensified – hospitals saw PPE waste explode, with one network’s glove usage doubling from 250,000 to 500,000 per day during surges.The pandemic highlighted how quickly disposable items can turn into mountains of costly waste. In summary, more disposable materials = more volume to dispose of, directly driving costs upward.
- Improper Segregation and Contamination of Waste Streams: Beyond the overuse of red bags, other segregation errors also raise costs. If hazardous waste is not separated from ordinary trash, it can contaminate entire waste streams, forcing more expensive handling. Conversely, hospitals miss out on cheaper diversion options if recyclables or compostables are thrown in regular trash.About 85% of hospital waste is non-regulated solid waste, and 60% of total hospital waste could be recyclable or composted. Failing to divert those materials means the hospital pays for landfill disposal unnecessarily (and loses potential recycling savings). Likewise, mixing sharps or infectious items into the wrong bin can trigger extra processing steps and fees for safety reasons. In short, when “what goes where” is not followed, the hospital pays more.
- Higher Regulatory and Compliance Costs: Handling medical waste requires strict regulations to protect public health and the environment. Non-compliance can result in hefty fines and legal costs, effectively increasing the overall cost of waste management. For instance, if a hospital disposes hazardous biomedical waste improperly, it may face penalties that add thousands of dollars to its monthly expenses.Interviews with environmental services directors at hospitals found that waste disposal mistakes led to fines of around $10,000 per month for some facilities. Even without penalties, increasing regulations often require more paperwork, specialized containers, training, and record-keeping – all of which entail costs. Waste disposal contractors have also raised prices in many regions, citing stricter disposal rules and higher treatment costs. The bottom line is that as regulations become more stringent, the cost of compliance (or failing to comply) is rising for hospitals.
- Growing Waste Volume per Patient: Healthcare services are expanding globally, and with them, waste output is growing. Studies have noted a correlation between higher healthcare spending and more waste generation.Simply put, more treatments, patients, and procedures mean more waste produced, from surgical drapes to food trays. In many countries, hospital waste volume (kg per bed) has increased yearly. Increased patient loads and service volumes directly translate to increased disposal costs without countermeasures.Specific departments are exceptionally high waste generators – for example, an analysis of a large Italian hospital found the operating theaters, intensive care units, and surgical wards produced the most hazardous waste per bed, driving up costs. As healthcare demands grow worldwide, hospitals face the challenge of managing waste streams that are larger than ever before, often with limited budgets.
Hidden Costs of Poor Waste Management
When hospital waste isn’t handled efficiently and correctly, the financial consequences exceed disposal fees. Some hidden costs and consequences of poor waste management include:
- Unnecessary Financial Waste: Money spent on excess waste disposal is not spent on patient care or facility improvements. Every dollar wasted on hauling away an improperly disposed item is a lost opportunity. For instance, consider that an overfilled red bag full of regular trash may cost 10 times more to dispose of than a black bag – that difference adds up to tens or hundreds of thousands of dollars over time, draining hospital resources. One case study showed that a 580-bed hospital saved $40,000 annually by eliminating disposable red bag liners and switching to reusable containers. This illustrates how addressing waste inefficiencies can free up significant funds.
- Regulatory Penalties and Legal Liability: Improper medical waste disposal can lead to fines, sanctions, or lawsuits. Environmental agencies routinely inspect healthcare facilities for compliance. A hospital that mixes sharps or infectious waste into general trash, or ships waste to an unapproved facility, risks severe penalties. These fines (which can reach thousands of dollars per violation) directly hit the hospital’s bottom line, effectively increasing the cost of waste management due to poor practices. In extreme cases, legal action or cleanup costs from an environmental incident (e.g., an infectious waste spill) can be hugely expensive. Thus, failing to manage waste properly can far exceed the cost of doing it right.
- Operational Inefficiencies and Labor Costs: Ineffective waste processes often result in workflow disruptions and extra labor hours. If waste containers are overfilled or misplaced, staff must take time away from patient duties to manage these issues. Missed pickups or miscommunication with waste vendors can further eat up staff time. In a survey of hospital environmental managers, many reported spending dozens of hours per month resolving waste problems – one group estimated around 50 hours/month were lost dealing with issues like overflowing bins or waste data tracking inefficiencies. Additionally, injuries or infections resulting from improper waste handling (e.g., needle-stick injuries to staff) can lead to lost work time and compensation costs. All these operational snags effectively act as hidden costs of poor waste management.
- Reputation and Environmental Impact: Healthcare institutions are expected to be stewards of public health and the environment. Improper waste disposal can damage a hospital’s reputation and community trust. For example, if biomedical waste is found in municipal landfills or (worse) in public areas due to mismanagement, the media and public outcry can be significant. Restoring public trust might require public relations efforts or community outreach – indirect costs stemming from a waste issue. Moreover, hospitals that do not prioritize sustainable practices may miss out on accreditation points or certifications (like LEED or Green Healthcare awards), which can have business and marketing implications. Finally, the environmental damage from excessive waste (overflowing landfills, higher carbon emissions from incineration, etc.) might not be billed to the hospital directly. Still, it contributes to broader healthcare costs (as pollution and poor environmental health ultimately create more disease and expense for society). In these ways, the cost of waste mismanagement is also paid in goodwill and ecological currency, not just dollars.
By recognizing these hidden costs, hospital administrators can strengthen the business case for investing in better waste management. The next section will explore exactly how to do that—by implementing strategies that reduce waste volumes, improve segregation, and ultimately slash the costs associated with hospital waste disposal.
Strategies to Reduce Hospital Waste Disposal Costs
The good news is that hospitals can take concrete steps to lower their waste management expenses without compromising on safety or compliance. Many cost-saving measures align with improved health outcomes and sustainability. Below are key strategies for reducing hospital waste disposal costs:
- Optimize Waste Segregation: Ensure that only actual medical/infectious waste goes into red biohazard containers and everything else goes into appropriate trash or recycling bins. This might mean placing RMW bins only where needed (e.g., in procedure rooms, not every patient room) and using clear labels and color codes. Proper segregation prevents paying exorbitant rates to dispose of what could be ordinary waste. Tip: Audit a few red bags to see if they contain regular trash – if so, there’s room to improve. Better segregation can yield immediate savings by avoiding the 10x higher cost of RMW disposal for non-hazardous items. Training staff on “what waste goes where” is critical (e.g., emphasize that paper towels or snack wrappers should never go in red bags). In one example, moving RMW bins out of public areas and closer to actual points of care cut down misclassified waste and saved significant costs.
- Educate and Train Healthcare Staff: Continuous education is one of the most effective tools to reduce waste mismanagement. All hospital personnel – doctors, nurses, janitorial staff, etc. – should know the proper waste disposal protocols. Common misconceptions (like “when in doubt, throw it in the red bag”) must be addressed. Encourage a culture where staff ask if uncertain and follow the waste management plan. Regular in-service training sessions, clear signage, and easy-to-follow guidelines help reinforce correct behavior. Over-classifying waste “just to be safe” is an expensive habit that training can correct. When everyone, from surgeons to housekeepers, understands improper waste disposal’s cost implications and environmental impact, they are more likely to follow procedures. Consider making waste reduction a part of performance improvement goals. Remember, a well-informed staff can dramatically reduce the volume of regulated waste and its associated costs.
- Use Reusable and Efficient Disposal Products: Hospitals can cut costs by switching from single-use waste containers and supplies to reusable alternatives where feasible. A prime example is sharps containers and medical waste bins – many facilities still use disposable plastic containers or liner bags that are thrown out with the waste. Not only do you pay to buy them continuously, but you also pay to dispose of them as medical waste. Studies show that roughly one-third of the “waste” in a medical waste bin can be the plastic container or liner itself, an avoidable cost. Hospitals eliminate that recurring expense by investing in reusable sharps containers and bin systems. These reusable systems can be safely emptied, sterilized, and returned to service. The upfront cost is offset by long-term savings on purchasing disposables and reduced waste volume. For instance, one large hospital that adopted a reusable RMW container system could eliminate red bag liners and save $40,000 in a year on bag purchase costs alone. Moreover, reusable products often have larger capacities or more efficient designs (e.g., no need for double packaging), reducing waste pickups and treatments. Go green to save green – reducing single-use plastics and switching to reusables is environmentally and financially savvy.
- Implement Recycling and Waste Reduction Programs: A significant portion of hospital “trash” – paper, cardboard, plastics, glass, even unused medical liquids – can often be recycled or composted at much lower cost than sending to a landfill or incinerator. Recycling reduces environmental impact and usually costs less per ton than general waste disposal, and certainly less than biohazard waste treatment. Identify materials in your waste stream that have recycling value: cardboard from supply deliveries, clean plastic packaging, beverage containers from the cafeteria, etc. A robust facility-wide recycling program can divert these items from the expensive waste routes. Likewise, explore composting for food waste from cafeterias and kitchens – food waste is heavy and unnecessarily drives up trash weight costs if not diverted. According to data, about 60% of a hospital’s waste could be recyclable or compostable with proper programs. By capturing that, hospitals can reduce waste volume (and cost) going to landfills or RMW processing. Some hospitals have also established reprocessing programs for unused medical supplies (certain unopened items can be re-sterilized or donated rather than trashed). Others engage in prevention initiatives, like more intelligent supply chain management to avoid over-ordering items that expire and go to waste. All these waste reduction efforts result in less tonnage that the hospital pays to haul away. Less waste generated equals lower disposal bills – it’s as simple as that.
- Conduct Regular Waste Audits and Monitoring: You can’t manage what you don’t measure. Performing periodic waste audits can uncover where waste management problems (and extra costs) arise. For example, an audit might reveal that a particular department (such as the Operating Room) is contributing a disproportionate amount of RMW, or that biohazard bins contain many non-hazardous items. Industry research indicates that operating rooms are often the worst offenders for tossing non-regulated waste into red bags due to the high-pressure environment and abundance of disposable supplies. Knowing this, a hospital could target OR staff for enhanced training or introduce specialized waste-sorting aides in surgery. Tracking waste generation by area or stream over time also helps quantify improvements. Many modern tools (even advanced software and IoT sensors) are available to help hospitals track fullness of bins, monitor segregation accuracy, and flag costly mistakes in real time. Even without high-tech solutions, establishing a routine audit (e.g., quarterly review of waste metrics) will show trends and let you address issues proactively. If you identify, say, that unused supplies worth $100,000 are being thrown out each year, you can take action to tighten inventory controls. Or if one ward’s recycling rate is low, you can focus efforts there. In summary, data-driven monitoring helps ensure your waste management plan stays on track and continuously improves, leading to sustained cost reduction.
- Ensure Compliance and Prepare for Regulations: Staying ahead of regulatory requirements can save money in the long run. This involves proper training (as mentioned), maintaining up-to-date waste management policies, and keeping documentation in order. If your facility handles special wastes (e.g., chemotherapy drugs, radioactive materials, or anatomical (body part) waste), make sure all legal protocols are followed so you don’t incur fines or emergency cleanup costs. Designating a Waste Compliance Officer or team that routinely checks that waste is being stored, labeled, and disposed of according to regulations may be worthwhile. Being proactive about compliance might involve some upfront effort and cost (for example, investing in a better autoclave or storage containers to meet new rules). Still, it prevents the far higher costs of violations. Additionally, many regions offer guidance or grants for healthcare waste reduction and sustainable practices – taking advantage of these can offset costs and improve compliance. Compliance is cheaper than non-compliance, and a well-run waste program keeps the hospital on the right side of the law and budget.
By implementing these strategies, hospitals can attack waste costs from multiple angles. Real-world results bear this out: improved segregation, education, and waste reduction initiatives have been shown to save facilities 40-70% of their waste disposal costs. Those savings can amount to millions of dollars system-wide or hundreds of thousands per hospital—funds that can go back into patient services or staff resources. Moreover, these steps have co-benefits: a cleaner environment, a safer workplace, and a positive reputation for sustainability.
Partnering with a Waste Management Expert for Cost Savings
Hospitals don’t have to tackle the waste challenge alone. One of the most effective ways to optimize waste management (and reduce costs) is to partner with a professional medical waste management service. Expert waste management companies bring specialized knowledge, tools, and services that can significantly ease the burden on hospital staff while cutting expenses. Here’s how an experienced waste management partner can help:
- Compliance and Safety: Professional providers stay current on all regulations and ensure your waste is handled and disposed of in full compliance with local and international laws. This minimizes the risk of costly fines or accidents. They also supply proper containers, labels, and transport, so you don’t have to invest separately.
- Cost Optimization: A good waste management partner will analyze your facility’s waste stream and help identify inefficiencies. They can recommend right-sizing services (e.g., adjusting pickup frequency or container types) so you’re not overpaying for unnecessary service. Many providers will assist with staff training on segregation and even perform waste audits for you, pinpointing where you can save money. Their expertise often leads to streamlined processes that lower your total cost of waste disposal.
- Sustainable Solutions: Leading waste companies offer options like waste-to-energy treatment, advanced recycling programs, or reusable container systems that a hospital might struggle to implement independently. By leveraging their infrastructure, hospitals can reduce environmental impact and potentially gain cost credits (for example, rebates for recycled materials or reduced fees for volume reduction initiatives).
- Convenience and Reliability: Managing medical waste internally can be complex and labor-intensive. Outsourcing to a trusted partner means your staff can focus on patient care while experts handle the waste logistics. The right partner will be reliable in pickups (no missed pickups that lead to overflow), responsive to emergency waste needs, and transparent in reporting. Over time, this reliability translates to fewer operational disruptions and more predictable costs.
In choosing a partner, hospitals should look for a provider with a strong track record in healthcare waste, proper certifications, and a commitment to safety and customer service. Getting a waste assessment or quote from the company is often beneficial to see potential savings and improvements outlined.
Secure Waste – Your Partner in Affordable Medical Waste Management
When it comes to managing and reducing the cost of medical waste disposal, Secure Waste is a leader in the field. Secure Waste offers comprehensive healthcare waste disposal and compliance solutions, helping hospitals and clinics handle everything from regulated medical waste and sharps to pathological and pharmaceutical waste safely and cost-effectively. With years of experience and a focus on efficiency, Secure Waste can design a waste management program tailored to your facility’s needs – often saving you money through better segregation protocols, optimized pickup schedules, and eliminating unnecessary waste services.
Secure Waste’s team of experts will work with your staff to ensure full compliance with all medical waste regulations (so you avoid costly fines) and provide ongoing support and education in best practices. Using modern treatment technologies and sustainable methods, Secure Waste helps healthcare facilities meet environmental goals while controlling costs. Many clients report significant reductions in their waste volume and disposal expenses after partnering with Secure Waste.
Ready to reduce your hospital’s waste management costs? Secure Waste can help you start with a free assessment and cost analysis. To learn more or to speak with a waste management expert, call Secure Waste at 877-633-7328. You can also visit their website at SecureWaste.net to request a quote or find more information about services. With the right partner and strategies in place, your hospital can turn the challenge of rising waste disposal costs into an opportunity for savings, safety, and sustainability.
By taking a proactive approach to hospital waste management – from segregating waste correctly to partnering with professionals – healthcare facilities around the globe can significantly curtail the escalating costs of waste disposal. The result is a leaner budget and a cleaner and safer healthcare environment for everyone. Investing in better waste practices today is an investment in your organization’s financial and environmental health for years to come.

Expert Medical Waste Management: With over 25 years of industry experience, Secure Waste is a trusted local leader in hazardous and biohazardous waste disposal across Maryland, Virginia, and Washington, D.C. Specializing in medical waste management, sharps needle disposal, and biohazard waste removal, the company ensures full compliance with federal, state, and local regulations while prioritizing environmental sustainability.
The company also offers additional services, including secure document shredding and sharps container sales, providing comprehensive solutions for healthcare facilities and businesses. Our cost-effective services help clients maintain regulatory compliance without unexpected costs.
With a commitment to customer satisfaction, Secure Waste offers tailored waste management plans that align with industry best practices. Their team of experts provides reliable, timely, and compliant services, making them the preferred choice for medical waste disposal. For a free waste quote or more information, visit www.securewaste.net