Staying Compliant With HIPAA Regulations With Digital Healthcare – Expert Healthcare Solutions With Secure Waste
Do you need help understanding HIPAA in the digital world?
Secure Waste, a local DMV company, emphasizes the challenges healthcare organizations face as patient communication increasingly shifts towards digital platforms and becomes instantly accessible via mobile devices.
The rise of electronic health records (EHRs), cloud-based storage solutions, remote access capabilities, and the use of third-party vendors has introduced a plethora of privacy and security risks that must be meticulously managed.
“Digital health platforms—whether offering AI-driven telehealth, remote monitoring, or patient portals—are often HIPAA-covered entities, business associates, or both.”
In this dynamic environment, safeguarding sensitive health data is more complex than ever. The Health Insurance Portability and Accountability Act (HIPAA) mandates strict guidelines for the protection of Protected Health Information (PHI), requiring organizations to maintain ongoing vigilance in their compliance efforts.
This includes regular assessments of their privacy policies and procedures, continual training for all staff on data security best practices, and active participation from every level of the organization, from management to frontline healthcare workers.
Moreover, failing to comply with HIPAA standards can be severe, leading to costly data breaches, regulatory fines, and a significant erosion of patient trust.
With the public increasingly aware of data privacy issues, maintaining effective HIPAA compliance is not just about adhering to legal requirements; it is a crucial investment in building and preserving a healthcare organization’s reputation.
By prioritizing PHI protection and fostering a culture of accountability, healthcare providers can mitigate risks and enhance the trust patients place in them.
Staying Compliant With HIPAA Regulations
Meeting the Challenges of HIPAA Compliance Today!
Welcome to Secure Waste, your premier partner in healthcare waste management serving Washington D.C., Virginia, and Maryland.
At Secure Waste, we are committed to providing exceptional Biomedical waste disposal services while embracing innovative solutions tailored for local healthcare providers. Our diverse clientele includes doctors, dentists, physicians, funeral homes, tattoo parlors, and many more, all entrusting us with their waste management needs.
In addition to our top-tier biomedical waste management and sharps disposal services, we support our partners in achieving compliance with the Health Insurance Portability and Accountability Act (HIPAA).
Ensuring HIPAA compliance is crucial, and clarity is one of the most critical factors. Policies and training programs that communicate requirements clearly tend to be more effective than those that are overly technical or confusing.
Although staff may need to temporarily shift their focus from patient care during training and policy updates, these efforts are vital components of a robust compliance program. To minimize any disruption to workflow, compliance resources must be efficient, accessible, and practical.

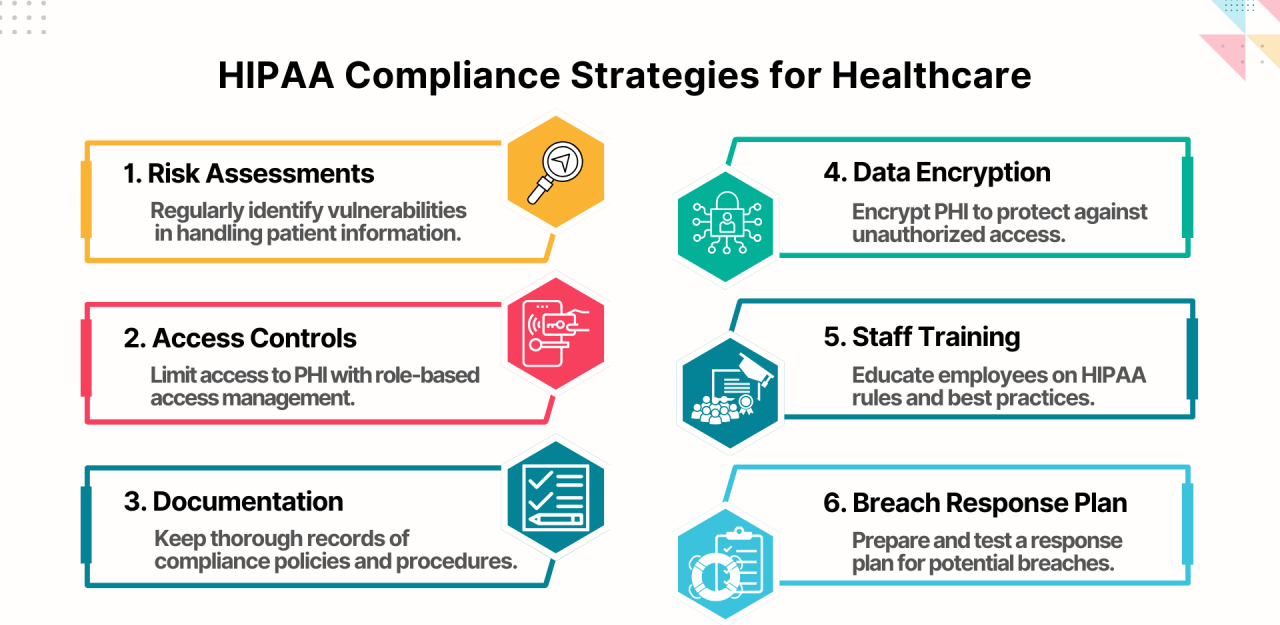
Here are key strategies healthcare organizations can employ to enhance and maintain strong HIPAA compliance:
1. Regularly Assess How Protected Health Information Is Shared
Before privacy or security gaps can be addressed, organizations must understand how PHI flows within and outside their networks. This includes identifying who has access to PHI, how information is transmitted, and when policies were last reviewed or updated. Rapid advancements in technology often mean existing safeguards may no longer be sufficient.
A structured HIPAA compliance assessment should include identifying internal departments, vendors, and business associates that receive or access PHI; reviewing current privacy and security policies for weaknesses or outdated practices; evaluating technical safeguards, such as access controls and encryption; and documenting all communication channels used to transmit PHI.
Conducting these assessments regularly—at least annually—helps ensure that new vendors, technologies, and workflows are appropriately evaluated and documented. Ongoing assessments also make it easier to track improvements and respond quickly to emerging risks.
2. Implement Risk Mitigation Strategies Based on Identified Gaps
Assessments often reveal vulnerabilities that require immediate attention. Once risks are identified, organizations should implement mitigation strategies to reduce the likelihood and impact of breaches. Standard measures include strengthening encryption protocols, updating social media and remote access policies, enhancing email security, and reinforcing identity verification procedures.
Employee training plays a critical role in risk mitigation. Staff should be trained to recognize phishing attempts, malware, and other cyber threats. Awareness programs that include simulated phishing exercises or periodic security reminders can significantly reduce human-error-related breaches.
HIPAA compliance is not limited to IT departments. Clinical staff, administrators, and support teams must all understand their responsibilities in protecting PHI. Collaboration across departments ensures policies are practical, realistic, and consistently followed. In some cases, consulting external HIPAA specialists can help organizations interpret regulatory guidance and develop stronger safeguards.
3. Establish a Clear and Detailed Breach Notification Plan
Even organizations with strong safeguards can experience data breaches. Industry data shows a sharp increase in healthcare data breaches over recent years, often involving large volumes of PHI. Breaches may result from simple mistakes, such as misdirected emails, or from sophisticated cyberattacks.
To respond effectively, organizations must have a documented incident response and breach notification plan. This plan should outline how incidents are identified, investigated, contained, and reported. Notification timelines, internal escalation procedures, and external reporting requirements should be clearly defined to ensure compliance with legal obligations.
Having a breach response plan in place helps reduce confusion during incidents, limits potential damage, and demonstrates due diligence during regulatory reviews.
4. Provide Ongoing HIPAA Training for All Employees
HIPAA requires organizations to train employees who handle or access PHI. Training should occur during onboarding and be reinforced regularly to keep policies and best practices top of mind. As regulations evolve and new threats emerge, refresher training becomes increasingly important.
Effective training programs account for varying roles, schedules, and learning preferences. Allowing staff to complete training at their own pace, offering role-specific content, and using real-world scenarios can improve engagement and retention. Training should emphasize practical actions employees can take to protect PHI in daily workflows.
Documenting training completion is also essential, as organizations must be able to demonstrate compliance during audits or investigations.
5. Prepare for Regulatory Updates and Policy Changes
HIPAA regulations continue to evolve alongside broader healthcare interoperability and patient access initiatives. Proposed updates to privacy rules aim to strengthen patient rights, improve data sharing for care coordination, and reduce barriers to accessing personal health information.
Healthcare organizations should monitor guidance from federal health authorities to stay informed about upcoming changes. Preparing early allows organizations to adjust policies, update forms, modify workflows, and train staff before new rules are enforced. Proactive preparation reduces disruption and minimizes compliance risk.
A Proactive Approach to HIPAA Compliance
HIPAA compliance is not a one-time effort. It requires continuous monitoring, training, assessment, and improvement. Organizations that embed privacy and security into daily operations are better positioned to adapt to regulatory changes and evolving threats.
While managing compliance internally can be challenging, many healthcare organizations choose to seek external expertise to support assessments, training, and policy development. Partnering with knowledgeable compliance professionals can help reduce administrative burden while strengthening overall program effectiveness.
By prioritizing data protection, investing in staff education, and maintaining clear response plans, healthcare organizations can safeguard patient information, reduce risk, and maintain trust in an increasingly digital healthcare environment.

Expert Medical Waste Management: With over 25 years of industry experience, Secure Waste is a trusted local leader in hazardous and biohazardous waste disposal across Maryland, Virginia, and Washington, D.C. Specializing in medical waste management, sharps needle disposal, and biohazard waste removal, the company ensures full compliance with federal, state, and local regulations while prioritizing environmental sustainability.
The company also offers additional services, including secure document shredding and sharps container sales, providing comprehensive solutions for healthcare facilities and businesses. Our cost-effective services help clients maintain regulatory compliance without unexpected costs.
With a commitment to customer satisfaction, Secure Waste offers tailored waste management plans that align with industry best practices. Their team of experts provides reliable, timely, and compliant services, making them the preferred choice for medical waste disposal. For a free waste quote or more information, visit www.securewaste.net






