Step By Step Guide For Proper Laundry And Linen Care For Hospitals And Surgery Centers: Expert Guide From Secure Waste
Healthcare Laundry Services: A Fresh Look
Laundry in healthcare facilities involves handling various items, such as bed sheets, blankets, towels, personal clothing, patient wear, uniforms, scrub suits, gowns, and surgical drapes, and even medical waste.
Although these textiles can potentially carry harmful microorganisms, relatively few documented healthcare-associated diseases are linked to contaminated laundry. As a result, the likelihood of disease transmission during the laundry process is considered relatively low.
In the United States alone, healthcare environments process approximately 5 billion pounds of laundry yearly. Established control measures—like standard precautions—are essential to reduce the risk of disease spread among patients and staff. Adhering to these guidelines effectively lessens the impact of contaminated laundry on the rates of healthcare-associated infections.
The guidelines governing healthcare facilities’ laundry services—whether in-house or outsourced—are based on hygiene principles, practical considerations, and consensus recommendations. Importantly, these guidelines specifically target laundry operations in healthcare settings, distinguishing them from laundry done at home.
What Does The Centers For Disease Control And Prevention (CDC) Say? “Click Here And See”

Healthcare Waste Management Secure Waste Solutions
Aspects Of Infection Control With Environmental Laundry Services in Healthcare
Contaminated textiles and fabrics can carry many microorganisms from bodily substances like blood, skin, stool, urine, vomit, and other fluids. These heavily contaminated items can have bacterial counts between 1 million (10^6) and 100 million (10^8) colony-forming units (CFU) for every 100 cm² of fabric.
Improper handling of contaminated fabrics, especially in healthcare settings, can spread diseases.
For instance, shaking soiled linens can release germs, including bacteria like Salmonella and Bacillus cereus, viruses such as hepatitis B, fungi like Microsporum canis, and parasites such as scabies. During sorting and handling, workers can be exposed to direct contact or airborne particles from contaminated lint.
Understanding that some infections might come from community sources, not just healthcare facilities, is essential. Effective cleaning methods can remove dirt and kill remaining pathogens to reduce risks, making the laundry hygienically clean. Properly cleaned textiles and clothing pose a very low risk to healthcare workers and patients, as long as the clean items are not contaminated again before use.
In the critical environment of healthcare facilities the effective management of linen is vital for preventing infections and ensuring patient safety This initiative focuses on best practices for handling transporting and laundering linens in hospitals across Maryland Virginia and Washington DC By implementing rigorous protocols and staff training these hospitals aim to minimize contamination risks maintain sterile environments and enhance overall infection control efforts This proactive approach protects patients and supports healthcare professionals in delivering high quality care
What Does OSHA Have to Say About Infection Control For Linens?
As defined by OSHA, contaminated laundry includes items soiled with blood or other potentially infectious materials, which may even contain sharps.
The primary focus of laundry guidelines is to protect workers from any exposure while collecting, handling, and sorting these items. Achieving this goal involves using appropriate personal protective equipment, implementing best work practices, effective containment methods, clear labeling, hazard communication, and ergonomic strategies.
By adhering to these standards, we can foster a safer and healthier work environment for everyone!
Whether healthcare workers should launder their uniforms at home has been a hot topic among experts.
OSHA regulations clearly state that home laundering of personal protective equipment is not allowed. However, there’s an ongoing dialogue about laundering uniforms and scrub suits that haven’t been contaminated with blood or infectious materials. It’s important to note that policies can vary across healthcare facilities and may not always match up with professional recommendations, creating uncertainty.
Interestingly, research indicates that uniforms without contamination may carry microbial risks comparable to regular street clothes, suggesting that home laundering could effectively sanitize them.
For facilities requiring uniforms, offering laundry services or providing precise guidance regarding best cleaning practices tailored to particular job functions is highly advisable.
A fascinating study of medical students’ white coats revealed some insightful findings.
Students considered their coats “clean” unless visibly soiled, even after frequent use.
The study highlighted the highest bacterial loads on the sleeves and pockets, mainly Staphylococcus aureus and other bacteria. Given that these areas come into contact with patients, they could spread microorganisms.
However, it’s worth noting that the study didn’t track any subsequent patient infections. The students said they would prefer to change their coats more often if clean alternatives were readily available.
On a broader scale, aside from the findings from this particular study, documented cases linking infections to healthcare clothing or home laundering practices are rare.
Healthcare laundry services can be structured in several ways: in-house (on-premise laundry), through cooperatives, or in partnership with off-site commercial laundry services. In off-site arrangements, healthcare facilities often own the linens and pay for laundering or opt to rent textiles from a provider.
Laundry facilities must comply with stringent design and operational standards to ensure hygienic textiles for patients and staff, especially in nursing environments. Typically, these facilities are organized into “dirty” and “clean” areas to minimize the risk of recontamination. The soiled laundry area must maintain negative air pressure compared to the clean section.
Accessible handwashing stations in laundry areas are essential, and staff must wear proper personal protective equipment when handling soiled items. Furthermore, following manufacturer guidelines is critical to maintaining equipment and preventing microbial contamination; leaving damp textiles in machines overnight is a practice to avoid.
By prioritizing these principles, we can collectively enhance hygiene and safety in healthcare settings, contributing to the well-being of patients and staff!

Working With Contaminated Textiles and Fabrics In Healthcare: No Easy Answers
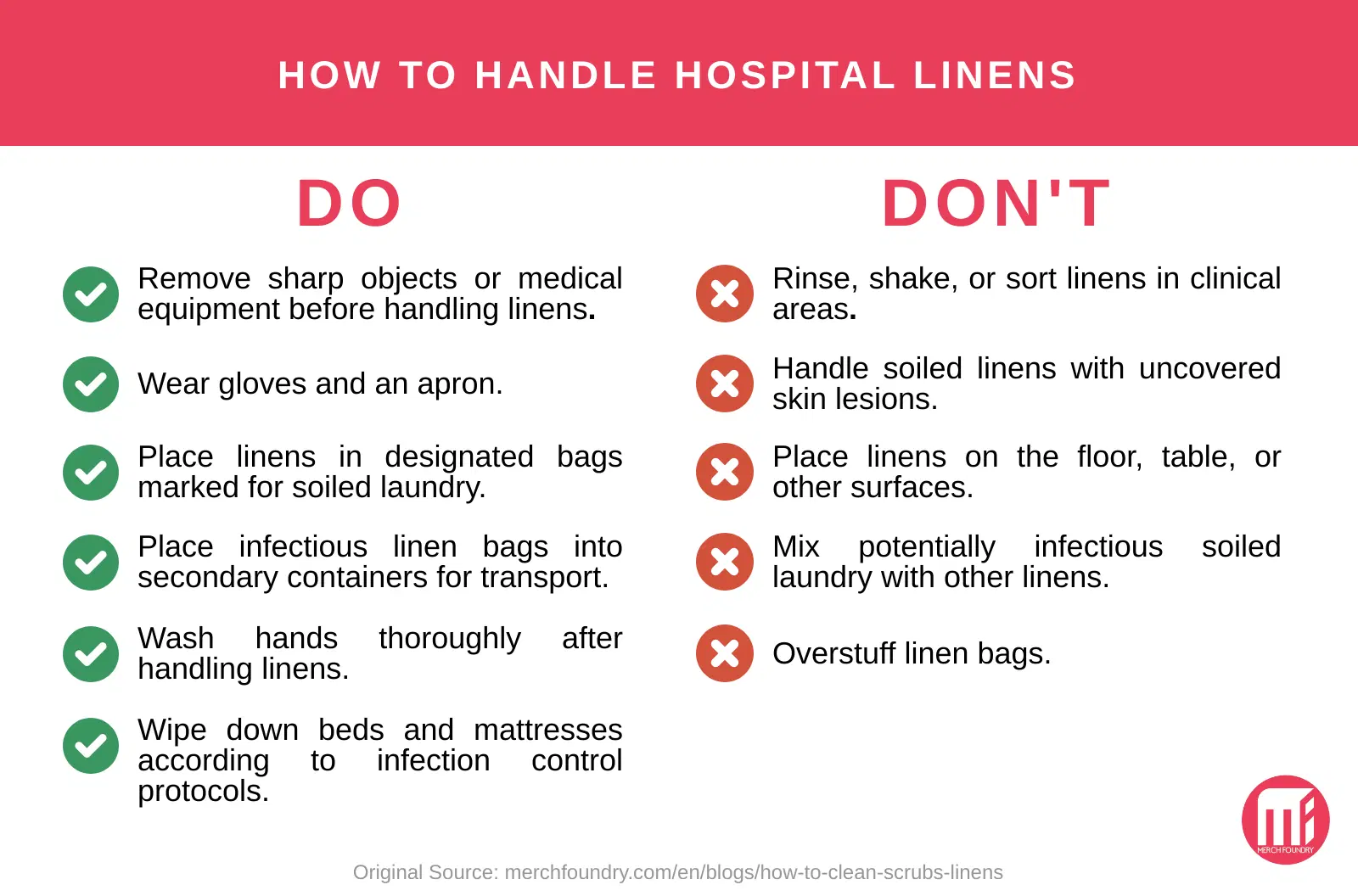
Proper laundry handling is crucial in healthcare settings to keep environments safe and clean. The process starts with carefully removing used or possibly contaminated items, like clothes and fabrics, from areas where contamination might happen, such as patient rooms and surgical areas.
Handling these items gently reduces agitation, which can create airborne lint in patient areas. OSHA regulations state that staff cannot sort or rinse contaminated laundry onsite, highlighting the importance of careful handling.
After collection, contaminated items are put in special bags or containers right where they were collected. These bags should be securely tied or sealed to avoid leaks. Leak-proof bags are necessary for safety, especially with wet laundry. Clear labels or color codes on these bags help healthcare workers handle them properly, whether moving them within the facility or sending them to an outside laundry service.
Laundry from isolation areas requires special handling. Studies show that laundry from these areas does not directly cause healthcare-associated infections. The contamination level in this laundry is often similar to that from other hospital areas. Following standard precautions and minimizing agitation of these items usually helps prevent the spread of infectious aerosols.
Carts or chutes can efficiently transport contaminated laundry. It’s essential to design, maintain, and use laundry chutes correctly. Keep chutes under negative air pressure to limit the spread of germs. Please don’t throw loose laundry into chutes, and always close laundry bags securely to avoid spills.
Healthcare facilities should decide when to sort textiles and fabrics during laundry. Sorting laundry after washing lowers staff exposure to infectious materials, reduces airborne germs in the laundry area, and prevents injuries. Sorting before washing protects workers and machinery from sharp objects like needles, reducing the risk of contaminating cleaned items.
Sorting before washing also allows for tailoring laundry processes based on the types of materials and soil present. An organized workflow separating different product types improves inspection, folding, and packing efficiency.
Appropriate protective gear must keep workers safe, and good ventilation must be ensured in the laundry area. When choosing gloves for sorting laundry, pick ones thick enough to protect against sharp injuries. Working with safety personnel and industrial hygienists can help find the best protective options for laundry staff.
By following these clear and proactive steps, we can create a safe and efficient laundry process that supports the health and safety of our healthcare environments. Let’s work together to enhance our procedures and show utmost care for patient care textiles.
The Laundry Process In Healthcare Settings: A Focused Review
Fabrics, textiles, and clothing used in healthcare settings are disinfected during laundering, making them hygienically clean but not sterile. Laundering includes flushing, main washing, bleaching, rinsing, and sorting. After cleaning, items are dried, pressed if necessary, and prepared for distribution.
When off-site laundries provide clean linens, they must be securely packaged to prevent contamination during transport. Effective packaging methods include:
- Using a hamper lined with a new liner that is closed or covered.
- Placing linens in a cleaned cart covered with disposable material or a cleaned reusable textile.
- Wrapping individual bundles in plastic or another suitable material and sealing them.
The antimicrobial effect of laundering results from mechanical, thermal, and chemical actions. Water agitation removes microorganisms, while soaps and detergents help suspend soils and have some antimicrobial properties. Effective hot-water washing typically requires at least 160°F (71°C) for 25 minutes. Chlorine bleach, activated at 135°F to 145°F (57.2°C to 62.7°C), is used for added safety, achieving a chlorine residual of 50–150 ppm. The final rinse often includes a mild acid to neutralize residual alkalinity, which helps inactivate some microorganisms.
While chlorine bleach enhances laundering, it is unsuitable for all fabrics, particularly traditional flame-retardant materials. However, some modern flame-retardant fabrics can tolerate it. Alternative laundry detergents, like activated oxygen-based products, offer antimicrobial benefits without compromising fabric safety. All products used in healthcare must be EPA-registered to ensure adequate disinfection. Healthcare workers should follow specific textile cleaning instructions to determine necessary laundering requirements.
Other Situations About Laundry And Linen Safety
Some textile items, like surgical drapes and reusable gowns, must be sterilized.
This is done through steam autoclaving after they are washed. Although the American Academy of Pediatrics once recommended autoclaving linens in neonatal intensive care units (NICUs), studies show that the cleanliness of regularly washed NICU linens does not increase the risk of infection for the babies cared for there. Therefore, clean linens are now considered safe for use in these units. However, whether sterile linens are necessary in burn therapy units is still debated.
Coated or laminated fabrics are often used to make personal protective equipment (PPE). Following the manufacturer’s cleaning instructions is vital when these items come into contact with blood or other bodily fluids. These guidelines take into account how the rubber backing interacts with cleaning chemicals. The item must be discarded if the backing shows signs of wear, like cracks.
Dry cleaning uses organic solvents like perchloroethylene to clean fabrics without damaging them.
However, relying solely on dry cleaning isn’t very effective in significantly reducing bacteria and viruses on dirty linens. Studies have shown that microbial levels drop significantly only after heat pressing dry-cleaned items. So, dry cleaning should not be considered the standard cleaning method for healthcare laundry and should only be used when fabrics can’t be safely cleaned with water and detergent.
A recent healthcare issue involves choosing between disposable (single-use) versus reusable (multiple-use) surgical gowns and drapes.
Regardless of the material, these items must resist liquids and germs. The FDA must approve surgical gowns and drapes to prove they are safe and effective. The fabric’s ability to repel liquids and its pore size affect performance, which is also influenced by the design and construction of the item.
Reinforced gowns with double layers are generally more resistant to liquids but may be less comfortable. Guidelines exist for choosing and using barrier materials for surgery. When selecting gowns and drapes, the level of liquid repellency must match the expected exposure.
However, there’s limited data about how gown or drape features affect the risk of surgical site infections. Healthcare facilities must ensure the safety of both patients and staff.
Not all fabric items in healthcare can be used just once. Facilities should weigh the cost of disposable items against the waste management costs after disposal. Using durable goods involves costs for the fabric, staff to manage laundry, and energy expenses for laundry services, whether in-house or contracted out.
Mattresses, Pillows, and More
Standard mattresses and pillows can become contaminated if their covers are damaged. Avoid using needles on mattresses, as a mattress cover protects against body fluids. A linen sheet is not a proper cover; torn covers should be replaced.
Stained or wet mattresses can harbor germs like Acinetobacter spp., MRSA, and Pseudomonas aeruginosa, which can infect vulnerable patients. Keeping mattress covers waterproof and clean is essential, and pillows should be washed between patients.
Air-fluidized beds are designed for patients with limited mobility and use warm air to keep tiny beads moving, preventing pressure sores. However, the beads can also become contaminated. Regular maintenance, cleaning, and replacing the polyester filter sheet are crucial to reduce the risk of germ spread. Beads should be heated to 113°F to 194°F for at least an hour to kill resistant germs like Enterococcus spp.
Despite the airflow, the germ levels around air-fluidized beds are similar to those around regular beds. Proper placement is necessary in negative-pressure rooms, so please consult a facility engineer for the best design.
In conclusion-
Now that you have a more comprehensive understanding of Infection control for laundry and linens in Hospitals and surgery centers, don’t hesitate to contact Secure Waste.
We provide reliable, compliant, eco-friendly medical waste disposal solutions for your facility’s needs. We have expertise in biomedical, hazardous waste, and Sharps container disposal. In addition, we provide customized waste management plans, including secure collection and transport, and sustainable disposal practices.
Contact us today for a FREE Waste Assessment, or request a quote online!

Expert Medical Waste Management: With over 25 years of industry experience, Secure Waste is a trusted local leader in hazardous and biohazardous waste disposal across Maryland, Virginia, and Washington, D.C. Specializing in medical waste management, sharps needle disposal, and biohazard waste removal, the company ensures full compliance with federal, state, and local regulations while prioritizing environmental sustainability.
The company also offers additional services, including secure document shredding and sharps container sales, providing comprehensive solutions for healthcare facilities and businesses. Our cost-effective services help clients maintain regulatory compliance without unexpected costs.
With a commitment to customer satisfaction, Secure Waste offers tailored waste management plans that align with industry best practices. Their team of experts provides reliable, timely, and compliant services, making them the preferred choice for medical waste disposal. For a free waste quote or more information, visit www.securewaste.net






