A Comprehensive Guide To Pathological Waste And Its Disposal For Surgery Centers
Pathological waste is a serious concern in surgery centers. According to the World Health Organization, pathological medical waste is classified as biomedical waste, posing significant risks of infection and contamination if mishandled. In the U.S. alone, healthcare facilities produce over 5.9 million tons of medical waste each year, a substantial portion of which is pathological.
Hence, proper segregation, storage, and disposal of pathological waste are not just regulatory requirements under OSHA and EPA guidelines but critical to patient and staff safety. In this guide, we’ll break down everything surgery centers need to know about managing pathological waste safely, legally, and efficiently, ensuring compliance and environmental responsibility.

In the bustling world of surgical centers efficient waste disposal is not just a necessityits a critical component of patient safety and environmental stewardship Every day these facilities generate various types of waste ranging from medical instruments to biohazard materials Ensuring that this waste is disposed of properly is crucial for maintaining a sterile environment and protecting the health of both patients and staff
What Is Pathological Waste?
Pathological waste is a specific category of biomedical waste that includes human or animal tissues, organs, body parts, and bodily fluids removed during surgeries, autopsies, or medical procedures. It is considered hazardous because it may contain infectious agents capable of spreading diseases.
Pathological waste is commonly generated in hospitals, laboratories, and veterinary clinics. Due to its biological origin and potential health risks, it requires strict handling, storage, and disposal procedures. Standard disposal methods include incineration or chemical treatment, ensuring compliance with health, safety, and environmental regulations to prevent contamination and disease transmission.
The Importance of Pathological Waste Management
Protects Public Health
Pathological medical waste can carry infectious agents like HIV, Hepatitis B and C, Mycobacterium tuberculosis, and other bloodborne pathogens. If tissues or body fluids are not properly disposed of, these pathogens can spread through contact or improper handling, leading to outbreaks or cross-contamination in healthcare settings and communities.
Reduces Environmental Pollution
When dumped in landfills or open areas, pathological waste decomposes and releases harmful biological matter into the environment, polluting natural resources and affecting wildlife and human populations.
Ensures Legal Compliance
EPA’s Medical Waste Tracking Act (U.S., 1988) mandates proper segregation, treatment, and disposal of pathological waste. Non-compliance can lead to heavy fines, criminal charges, or shutdowns of healthcare facilities. These legal frameworks also cover protocols for proper pharmaceutical waste management and sharps needle disposal during surgery.
Protects Healthcare Workers and Waste Handlers
The WHO reports that 15% of healthcare waste is considered hazardous, and needle-stick injuries from waste are a leading cause of occupational exposure to disease. Implementing best practices for sharps disposal in Virginia and Maryland, along with using PPE and safety containers, drastically minimizes risks for frontline medical personnel.
Prevents Spread of Drug-Resistant Pathogens
Improper disposal of pathological waste has been linked to the spread of antimicrobial-resistant bacteria in the environment. A WHO study highlights poor pathological waste disposal as a factor in rising global antimicrobial resistance (AMR). If waste containing drug-resistant microbes isn’t treated effectively, these organisms can enter water and soil, making infections more challenging to treat and increasing global health threats.
Supports Public Trust in Healthcare Systems
Visible cleanliness and hygiene practices, including proper pathological waste management, influence patients’ trust in healthcare facilities. When the public sees biohazard waste disposed of safely and professionally, it builds confidence in medical institutions and reduces fear of exposure or mistreatment.
Segregation and Disposal of Pathological Waste
Segregation Guidelines
As per the WHO, waste should be segregated at the point of generation (i.e., where it is produced). As per biomedical waste disposal rules, you are required to use color-coded bins:
- Yellow container/bag for pathological waste (tissues, organs, body parts).
- Bags should be non-chlorinated plastic and clearly labeled as biohazardous.
- Double-bagging is recommended for large or moist tissue waste to prevent leakage.
Proper segregation also includes separating sharps into puncture-proof containers to meet the sharps disposal requirements in Maryland and Virginia.
Handling and Storage
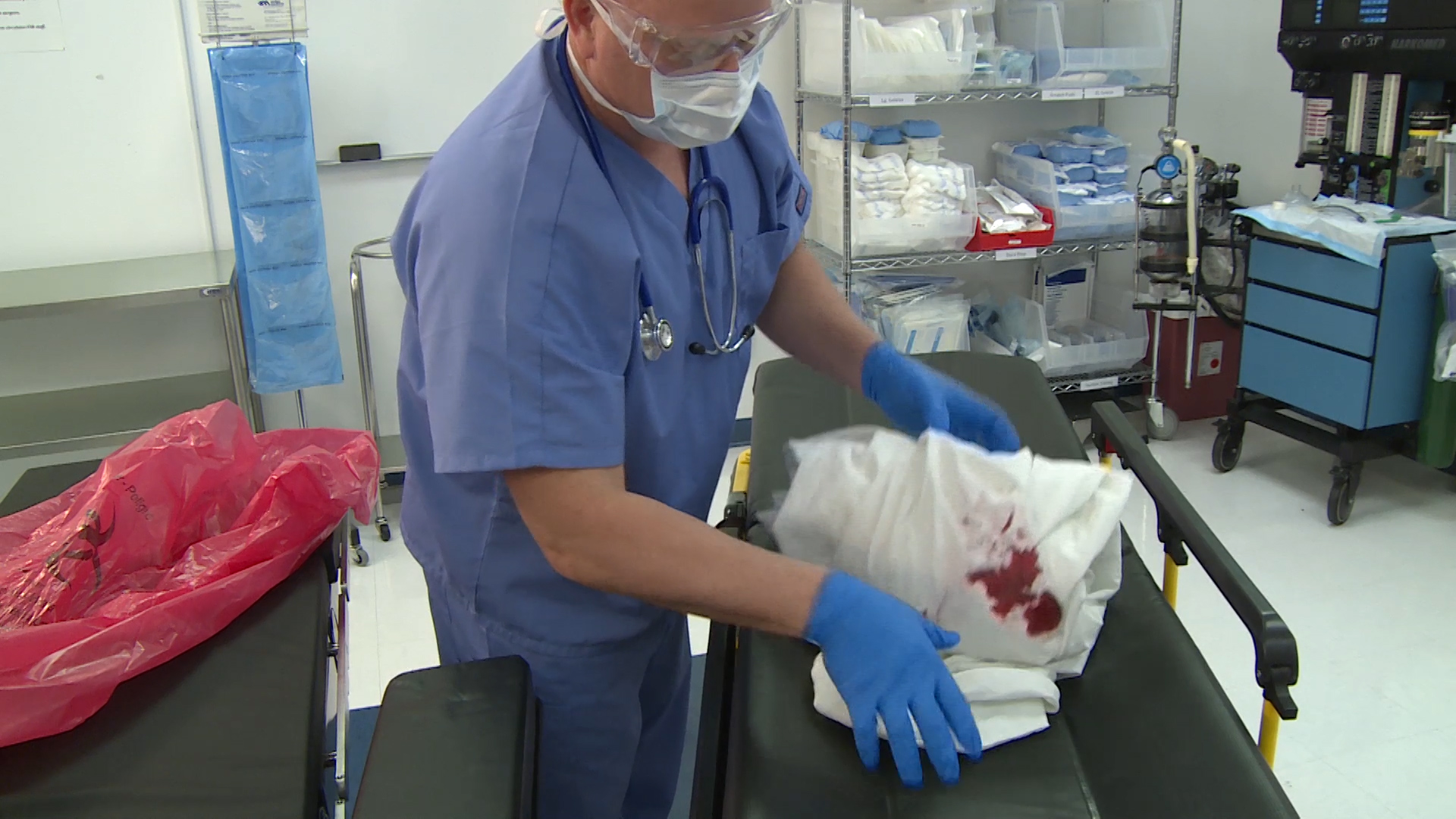
- Should be handled with personal protective equipment (PPE) – gloves, gowns, masks, and goggles.
- Must be stored in leak-proof, sealed containers.
- Should be stored in cold rooms (below 4°C) if not treated within 24 hours.
- Kept in restricted access areas to avoid unauthorized contact.
Transportation
- Transported in dedicated, labeled, and leak-proof vehicles.
- Should follow the “cradle-to-grave” principle–tracking waste from generation to final disposal.
- Transport containers must have biohazard symbols and follow local transportation regulations.
Disposal Methods
There are four standard Pathological Waste disposal methods:
Incineration
Incineration is a standard method for pathological medical waste disposal. It involves high-temperature combustion, typically above 850°C. This process effectively destroys organic matter, tissues, and pathogens, reducing the waste to ash and minimizing its infectious potential. However, a significant drawback of incineration is the potential release of toxic air pollutants, such as dioxins and furans, primarily if the incineration process is not managed correctly with pollution control technologies. Therefore, regulatory oversight is essential to ensure environmental compliance.
Deep Burial
It is a traditional and cost-effective method used primarily in rural or remote areas where access to incineration or other advanced disposal technologies is unavailable. It involves placing pathological waste into typically 2 to 3 meters deep pits, ensuring that the burial site is far from water sources to prevent groundwater contamination. After the waste is deposited, the pit is covered with lime and soil, which acts as a disinfectant and also helps deter animal scavenging.
Alkaline Hydrolysis (Advanced Method)
It uses a strong alkaline solution (usually potassium or sodium hydroxide) combined with high pressure and elevated temperatures to break down biological materials into a sterile liquid and soft tissue residue. This method is highly effective and produces no harmful emissions like incineration does.
Autoclaving/Steam Sterilization
Autoclaving is a standard sterilization method that uses pressurized steam to kill pathogens in medical waste. However, it is generally ineffective for pathological waste, especially with high organic content such as tissues and body parts. The method is much more suitable for microbiological waste, like culture media and lab instruments, where the primary concern is disinfection rather than volume reduction or destruction of organic tissue.
Record-Keeping and Monitoring
Healthcare facilities must maintain thorough waste generation, transport, and disposal records for regulatory audit trails (supported under RCRA “cradle-to-grave” principles).
- Periodic audits and inspections are necessary to ensure adherence.
- Compliance with OSHA, DOT, CDC, EPA (federal), and state policies is essential; failure can result in severe fines (up to tens of thousands USD per violation) or permit loss
- The use of barcoding and GPS tracking is becoming more common in monitoring waste movement.
- Staff must be trained regularly on pathological waste management, including PPE use, segregation, emergency response, and sharps needle disposal procedures.
Conclusion
Cutting corners isn’t an option when handling pathological and medical waste; your patients, staff, and community depend on you. That’s where Secure Waste comes in. We’re not just another waste hauler but your committed partner in medical waste disposal, offering compliant, safe, and hassle-free solutions tailored for your facility. Whether it’s pathological waste, pharmaceutical waste, or sharps disposal in Maryland or Virginia, we’ve got you covered. Let us handle the waste, so you can focus on what truly matters, caring for lives.

Expert Medical Waste Management: With over 25 years of industry experience, Secure Waste is a trusted local leader in hazardous and biohazardous waste disposal across Maryland, Virginia, and Washington, D.C. Specializing in medical waste management, sharps needle disposal, and biohazard waste removal, the company ensures full compliance with federal, state, and local regulations while prioritizing environmental sustainability.
The company also offers additional services, including secure document shredding and sharps container sales, providing comprehensive solutions for healthcare facilities and businesses. Our cost-effective services help clients maintain regulatory compliance without unexpected costs.
With a commitment to customer satisfaction, Secure Waste offers tailored waste management plans that align with industry best practices. Their team of experts provides reliable, timely, and compliant services, making them the preferred choice for medical waste disposal. For a free waste quote or more information, visit www.securewaste.net