Bloodborne Pathogens in Healthcare: Risks and Prevention
Secure Waste, a trusted local biomedical waste and sharps management company, specializes in the safe and compliant handling of infectious materials, including bloodborne pathogens.
With years of experience in the field, we have developed a thorough understanding of best practices in healthcare waste management and safety protocols. Our dedicated team is trained to follow all applicable federal and state regulations, ensuring the proper disposal of biomedical waste and reducing potential risks to public health and the environment.
If you need reliable biomedical waste disposal services in Maryland, Virginia, or Washington, D.C., please get in touch with Secure Waste at 877-633-7328.
Our skilled staff is ready to help you with tailored solutions that meet your facility’s specific needs. In the meantime, let’s explore some key insights and guidelines that can enhance your understanding of healthcare waste management practices.

Bloodborne Pathogens in Healthcare: Risks and Prevention
Bloodborne pathogens are a significant occupational hazard in healthcare environments.
These microorganisms, which include certain viruses and bacteria found in blood and specific bodily fluids, have the potential to cause severe disease when transmitted from one person to another.
Because healthcare workers routinely perform tasks that involve contact with blood or other potentially infectious materials, exposure risks must be actively managed through the implementation of structured controls and adherence to regulatory compliance.
Understanding bloodborne pathogens and how to prevent exposure is essential for protecting healthcare employees, patients, and the broader community. A comprehensive approach combines education, engineering controls, work practice controls, and clearly defined response procedures. When these elements work together, organizations can significantly reduce exposure incidents and maintain regulatory alignment.
What Are Bloodborne Pathogens
Bloodborne pathogens are microorganisms present in human blood that can cause disease when transmitted through exposure to contaminated blood products or bodily fluids.
Some of the most commonly recognized bloodborne pathogens include the human immunodeficiency virus (HIV), hepatitis B virus, and hepatitis C virus. These pathogens can be transmitted through contact with infected blood or certain bodily fluids entering the body through cuts, puncture wounds, or mucous membranes.
Healthcare workers face heightened exposure risks because of the nature of their work. Procedures involving needles, scalpels, and other sharps increase the likelihood of percutaneous injuries.
Exposure may also occur when blood or infectious fluids come into contact with the eyes, nose, mouth, or broken skin. Without proper safeguards, these exposures can lead to serious and sometimes life-altering health consequences.
How Exposure Occurs in Healthcare Settings
Exposure to bloodborne pathogens most commonly occurs through needlestick injuries or cuts from contaminated sharps.
These incidents can occur during procedures, the disposal of sharps, or the improper handling of waste.
Contact with blood or infectious fluids can also arise during patient care activities, laboratory work, cleaning tasks, or the handling of waste.
In many cases, exposure incidents can be prevented. Lack of proper protective equipment, inadequate training, rushed workflows, and poorly designed disposal systems all increase risk. Recognizing common exposure scenarios allows organizations to create targeted controls that address real-world hazards.
OSHA’s Role in Protecting Healthcare Workers
The Occupational Safety and Health Administration establishes requirements to protect employees who may reasonably anticipate contact with blood or other potentially infectious materials as part of their job duties.
These requirements form the foundation of bloodborne pathogen safety programs in healthcare settings.
OSHA standards require employers to implement measures that reduce exposure risk and provide appropriate follow-up care in the event of exposure.
These measures include written exposure control plans, training, engineering controls, and access to protective equipment. Compliance with these standards is mandatory and applies to hospitals, clinics, laboratories, dental offices, veterinary practices, and other workplaces where there is a risk of exposure to bloodborne pathogens.
Core Elements of Bloodborne Pathogen Controls
Effective bloodborne pathogen prevention relies on multiple layers of protection. Engineering controls are designed to remove or isolate hazards and include sharps containers, needleless systems, and safer medical devices.
These controls reduce reliance on individual behavior and help prevent injuries before they occur.
Work practice controls focus on how tasks are performed.
Examples include proper hand hygiene, safe handling of sharps, and procedures for cleaning and decontamination. When employees consistently follow established practices, exposure risks decrease significantly.
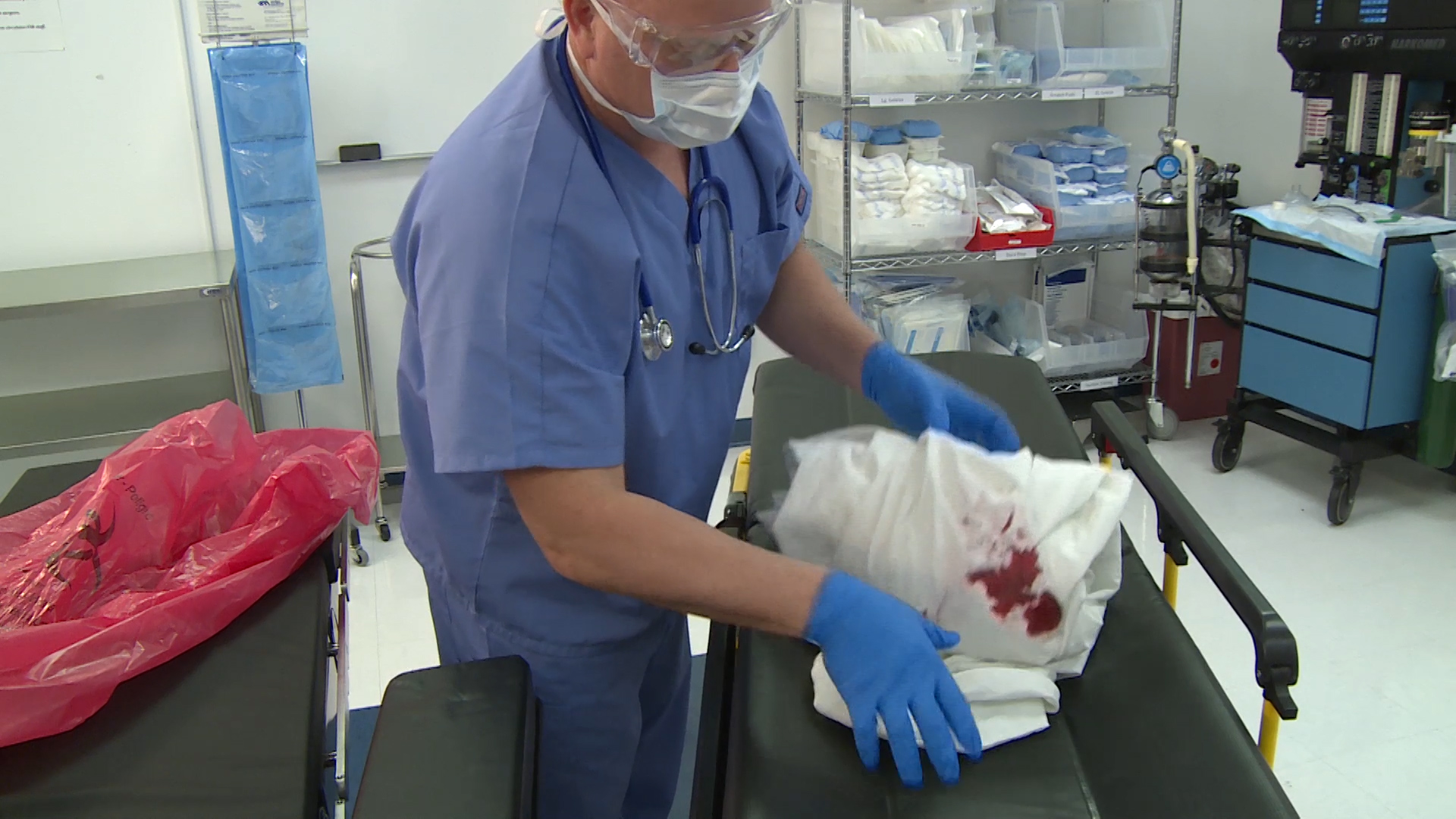
Personal protective equipment provides a barrier between workers and infectious materials, thereby protecting them from potential exposure to these materials. Gloves, masks, gowns, and eye protection must be readily available, appropriately sized, and used correctly.
PPE is most effective when combined with engineering and work practice controls, rather than relying solely on it.
Training as a Critical Compliance Requirement
Training is a cornerstone of bloodborne pathogen prevention. Employees who are at risk of exposure must receive initial training and regular refresher education that explains hazards, protective measures, and response procedures.
Training should be practical, role-specific, and easy to understand.
Practical training helps employees recognize exposure risks and understand their responsibilities. It also reinforces proper use of equipment and procedures, reducing the likelihood of unsafe practices. Documentation of training completion is essential for demonstrating compliance during inspections or audits.
The Importance of an Exposure Control Plan
A written exposure control plan is required for organizations with occupational exposure risks.
This plan outlines how exposure will be prevented and how the organization will respond in the event of an incident. It should identify job classifications with exposure risk, describe control measures, and detail post-exposure evaluation and follow-up procedures.
Exposure control plans must be reviewed and updated regularly to reflect changes in tasks, equipment, or regulations. An outdated plan can create gaps in protection and increase liability.
Keeping the plan current ensures that employees know exactly what to do if exposure occurs and that organizations remain prepared for regulatory review.
Response and Follow-Up After Exposure
Despite preventive efforts, exposure incidents may still occur. Prompt response is essential to reduce health risks and ensure compliance.
Employees should know how to report exposures immediately and where to seek medical evaluation.
Post-exposure procedures typically include documentation of the incident, medical evaluation, and follow-up care as recommended by healthcare professionals. Clear reporting pathways and supportive policies encourage timely reporting, reducing the likelihood of unaddressed incidents.
The Role of Waste Management in Exposure Prevention
Improper waste handling is a major contributor to bloodborne pathogen exposure. Sharps and contaminated materials must be disposed of in appropriate containers designed to prevent punctures and leaks.
Waste should be segregated correctly and removed in accordance with regulatory requirements.
Partnering with an experienced waste management provider supports safe disposal practices and reduces exposure risks. Secure Waste collaborates with healthcare organizations to deliver compliant sharps and medical waste solutions that safeguard staff and ensure OSHA compliance. Learn more with Secure Waste.
Building a Culture of Safety and Accountability
Bloodborne pathogen prevention is most effective when supported by a strong safety culture.
Leadership commitment, clear communication, and employee engagement are essential components of effective management.
When safety is prioritized at every level, compliance becomes part of daily operations rather than a reactive obligation.
Encouraging reporting, recognizing safe behaviors, and addressing hazards promptly reinforces accountability and promotes a culture of safety. Over time, this culture reduces incidents, improves morale, and strengthens organizational resilience.
Long-Term Benefits of Proactive Compliance
Organizations that invest in proactive bloodborne pathogen controls benefit from fewer injuries, reduced absenteeism, and stronger regulatory standing.
Consistent compliance also protects reputation and builds trust with patients, staff, and the community.
By integrating training, planning, and proper waste management into daily workflows, healthcare organizations create safer environments and support long-term operational success.
Final Takeaway
Bloodborne pathogens pose a significant risk in healthcare environments; however, exposure can be prevented primarily through the implementation of adequate controls and compliance.
Understanding how pathogens are transmitted, implementing OSHA-required protections, maintaining an up-to-date exposure control plan, and ensuring proper waste disposal are essential steps in protecting workers. A proactive, well-structured approach safeguards employee health, supports regulatory compliance, and reinforces a culture of safety that benefits everyone involved.

Expert Medical Waste Management: With over 25 years of industry experience, Secure Waste is a trusted local leader in hazardous and biohazardous waste disposal across Maryland, Virginia, and Washington, D.C. Specializing in medical waste management, sharps needle disposal, and biohazard waste removal, the company ensures full compliance with federal, state, and local regulations while prioritizing environmental sustainability.
The company also offers additional services, including secure document shredding and sharps container sales, providing comprehensive solutions for healthcare facilities and businesses. Our cost-effective services help clients maintain regulatory compliance without unexpected costs.
With a commitment to customer satisfaction, Secure Waste offers tailored waste management plans that align with industry best practices. Their team of experts provides reliable, timely, and compliant services, making them the preferred choice for medical waste disposal. For a free waste quote or more information, visit www.securewaste.net