The World Health Organization estimates that only about 15% of healthcare waste is hazardous, yet that small fraction accounts for nearly all the risk, costs, and regulatory scrutiny. When it is mismanaged, the consequences are immediate and severe.
In the United States, compliance is especially complex. Since federal oversight ended with the expiration of the Medical Waste Tracking Act, medical waste has been regulated primarily at the state level. Each state now defines, tracks, stores, and treats regulated medical waste differently. In 2026, this patchwork of rules is tighter than ever, with strict time limits, manifest requirements, and treatment mandates such as autoclaving or incineration.
This guide provides a clear, authoritative roadmap to medical waste disposal and regulatory compliance, what qualifies as regulated medical waste, how federal and state rules interact, where facilities fail, and how to build a compliant, defensible program.
What Qualifies as Medical Waste?
1. Sharps
Items capable of puncturing skin and causing injury:
- Needles and syringes
- Scalpel blades
- Lancets
- Broken glass from laboratories
- Contaminated slides and pipettes
| The Centers for Disease Control and Prevention (CDC) estimates that hospital-based healthcare workers experience roughly 385,000 needlestick and sharps-related injuries each year in the United States. Sharps represent the highest injury risk and must be discarded immediately in puncture-resistant containers at the point of use. |
2. Blood and Body Fluids
Materials saturated or dripping with:
- Blood
- Plasma or serum
- Suction canister contents
- Dialysis waste
- Pathology specimens
3. Microbiological and Laboratory Waste
Includes materials contaminated with microorganisms, such as:
- Cultures and stocks of microorganisms
- Petri dishes and culture plates
- Live vaccines
- Waste from isolation labs
These wastes pose the greatest infection risk and are typically required to be treated on-site or through certified healthcare waste disposal methods.
4. Pathological and Anatomical Waste
Includes human and animal tissues such as:
- Tissues
- Organs
- Body parts
- Biopsy specimens
5. Pharmaceutical and Chemical Waste
- Expired or unused medications
- Chemotherapy agents
- Formaldehyde, solvents, reagents
- Mercury-containing devices
Some pharmaceuticals are classified as hazardous waste under RCRA and must be managed separately.
6. Radioactive Waste
Materials contaminated with radionuclides from:
- Nuclear medicine
- Oncology treatments
- Research laboratories
7. APHIS-Regulated Waste (USDA)
Facilities working with animals or agricultural pathogens generate waste governed by the USDA’s Animal and Plant Health Inspection Service. This includes infected animal tissues, bedding, cultures, and disposable PPE from quarantine or high-containment areas. APHIS waste is controlled by federal permits and often requires on-site treatment, secured movement, and approved destruction methods.
OSHA Compliance for Medical Waste
The Occupational Safety and Health Administration (OSHA) is a federal agency under the U.S. Department of Labor, established in 1970 to ensure safe and healthy working conditions across all industries. OSHA develops and enforces standards, provides training, and promotes workplace safety to prevent occupational injuries, illnesses, and fatalities. In healthcare, OSHA’s mission includes protecting employees from exposure to biological hazards and other risks associated with medical waste.

Protecting Workers Handling Medical Waste
Healthcare facilities generate materials that may contain bloodborne pathogens or other infectious agents. OSHA requires organizations to implement exposure control plans, provide engineering and work-practice controls, and ensure proper use of personal protective equipment (PPE). Universal precautions dictate that all blood and potentially infectious materials (OPIM) be treated as hazardous, regardless of visible contamination.
Bloodborne Pathogens and Safe Waste Management
The Bloodborne Pathogens Standard (29 CFR 1910.1030) sets requirements for handling sharps, contaminated PPE, and other medical waste. Facilities must use puncture-resistant, leak-proof containers, label all biohazard materials clearly, and train staff in spill response and post-exposure procedures. Regular refresher training keeps employees aware of evolving risks.
Documentation, Compliance, and Safety Culture
OSHA emphasizes meticulous recordkeeping, including training logs, exposure incidents, and vaccination records. Integrating OSHA guidance with CDC infection-control protocols and EPA disposal regulations ensures comprehensive safety. Supervisors must monitor compliance, enforce procedures, and maintain secure storage and transport, fostering a culture of accountability and risk reduction.
By following OSHA standards, healthcare organizations protect staff, reduce pathogen exposure, and remain compliant with federal and state regulations governing medical waste disposal.
HIPAA Compliance in Medical Waste Management
HIPAA requires that any item containing protected health information (PHI) be disposed of in a way that makes it completely irretrievable. Even something as small as a prescription label or lab report can trigger a violation if mishandled.
Medical waste programs that fail to address PHI exposure put facilities at risk of fines, legal action, and loss of patient trust. A compliant system ensures that privacy is preserved from the moment waste is generated to its final destruction.
Protecting PHI Through Secure Waste Disposal
Medical waste often contains more than contaminated materials. It can also expose sensitive data, including:
- Prescription bottles and medication labels
- Lab results and diagnostic reports
- Patient charts and identifiers
- Any paper or item displaying PHI
| In a related study by The HIPAA Journal, researchers found approximately 2,867 documents containing personally identifiable information (PII) incorrectly placed in recycling streams and 1,885 items containing protected health information (PHI) discarded in general waste bins, highlighting how easily privacy breaches occur through improper medical waste disposal. |
Best Practices Include:

Secure Document & Media Destruction
HIPAA applies to both physical and digital records. Paper files, X-rays, USB drives, and copier hard drives all require secure destruction. Acceptable methods include:
- Cross-cut or micro-cut shredding for documents
- Pulping or incineration for high-volume waste
- Physical destruction or degaussing for electronic media
Facilities should also maintain:
- Locked collection containers in every department
- Scheduled destruction intervals to avoid buildup
- Certificates of destruction from vendors
- Logs documenting date, method, and handler
Dual Compliance: OSHA + HIPAA
OSHA focuses on worker safety. HIPAA focuses on patient privacy. A compliant waste program must satisfy both.
A dual-compliant system ensures:
- Regulated medical waste is contained, labeled, and handled safely (OSHA)
- PHI is separated, secured, and destroyed beyond recovery (HIPAA)
- Staff are trained on both exposure prevention and privacy protection
- Chain-of-custody documentation exists from pickup to destruction
DOT & Transportation Requirements
Transporting medical waste is regulated by the U.S. Department of Transportation (DOT) to protect workers, the public, and the environment. From the moment waste leaves a facility, it must meet strict federal standards for packaging, labeling, and carrier handling.
DOT’s Role in Hazardous Waste Transport
DOT governs how hazardous and regulated medical waste is prepared and moved on public roads. These rules ensure that garbage is:
- Packaged in approved, leak-proof containers
- Labeled with proper hazard markings and identification numbers
- Transported by carriers certified to handle hazardous materials
Facilities are responsible for preparing waste correctly before pickup. Carriers are responsible for maintaining compliance during transport. Any failure, be it improper packaging, missing labels, or uncertified drivers, can result in violations, delays, and significant fines. DOT compliance ensures that waste remains contained, traceable, and safe from pickup to final medical waste disposal.
DOT Packaging Groups

Hazardous Materials Identification
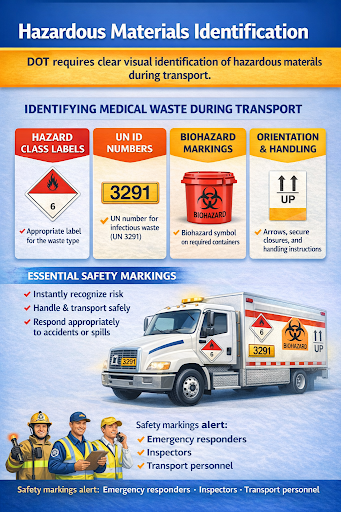
Accurate labeling is not optional. It is a core safety measure that protects drivers, dock workers, first responders, and the public while maintaining full regulatory compliance.
Federal Regulations Governing Medical Waste
EPA Guidelines
The Environmental Protection Agency (EPA) focuses on the environmental impacts of medical waste, emphasizing prevention, safe handling, and responsible disposal.
Waste Minimization
The EPA encourages healthcare facilities to reduce waste at the source. This includes:
- Choosing reusable or lower-volume products when possible
- Segregating regulated medical waste from general trash to avoid over-classification
- Implementing recycling programs for non-contaminated materials
Environmental Handling Regulations
EPA guidance supports treatment methods that neutralize hazards while limiting environmental harm. These include:
- Autoclaving (steam sterilization)
- Chemical treatment
- Approved incineration systems that meet air-quality standards
Medical Waste Tracking Act
The Medical Waste Tracking Act (MWTA) was enacted in 1988 after medical debris washed up on U.S. beaches, raising public alarm. The law established a federal demonstration program that tracked medical waste from generation to disposal in select states.
Purpose and History
Although the MWTA expired in 1991, it left a lasting framework that continues to shape modern medical waste regulation. Its key contribution was the concept of cradle-to-grave accountability, the idea that waste generators remain responsible for their waste until final medical disposal.
Today, most states base their tracking and compliance systems on this model, requiring:
- Proper packaging and labeling
- Documented transfer between parties
- Verifiable treatment and destruction
The MWTA set the standard for traceability that remains central to compliant waste management.
APHIS / USDA Regulations
The Animal and Plant Health Inspection Service (APHIS), under the U.S. Department of Agriculture (USDA), regulates waste associated with animal health, agriculture, and biological research.
When APHIS Applies
APHIS oversight is required when medical or biological waste involves:
- Animal research facilities
- Veterinary clinics and laboratories
- Pathogens or materials that could impact livestock, crops, or ecosystems
- Imported biological agents or animal products
Internal Facility Procedures & Best Practices
Waste Segregation
Key practices include:
- Separate regulated medical waste from general trash – only items that meet the definition of medical waste should go into designated containers.
- Differentiate waste types – There should be separate containers for sharps, infectious waste, trace chemotherapy, and pharmaceutical waste management.
- Train staff on identification – clear examples and regular refresher training help prevent accidental misclassification.
- Avoid over-classification – not all trash from clinical areas is regulated; unnecessary disposal as medical waste increases cost and processing burden.
Labeling & Containers
Correct labeling and container selection are critical to safety and compliance:
- Use puncture-resistant, leak-proof containers for sharps – must remain upright and not overfilled.
- Clearly label containers – include the universal biohazard symbol or use red-colored containers for easy identification.
- Lockable containers for PHI or confidential materials – prevent unauthorized access and ensure HIPAA compliance.
- Color coding and signage – helps staff quickly identify container purpose and waste type.
Storage & Handling
Proper storage and handling minimize exposure risks and maintain compliance with OSHA, EPA, and state regulations:
- Secure storage areas – medical waste should be kept in locked or restricted-access locations until collection.
- Secondary containment – required if there is a risk of leakage during storage or transport.
- Safe handling practices – train staff on lifting, transporting, and transferring containers to reduce injury risk.
- Routine inspections – verify container integrity, label accuracy, and adherence to storage requirements.
Infection Control & Risk Reduction
Effective infection control and risk reduction are essential components of medical waste management. Key practices include:
- Hand Hygiene – Wash hands thoroughly before and after handling medical waste to prevent pathogen spread.
- Personal Protective Equipment (PPE) – Use gloves, gowns, masks, and eye protection appropriate for the waste type.
- Safe Sharps Handling – Dispose of needles and other sharps immediately in approved puncture-resistant containers.
- Proper Segregation – Separate infectious waste from general and non-regulated waste to minimize cross-contamination.
- Surface Disinfection – Regularly clean and disinfect work surfaces, carts, and storage areas.
- Spill Response – Have clear protocols for containing, cleaning, and disposing of spills safely.
- Employee Training – Provide ongoing education on infection control practices, proper waste handling, and emergency procedures.
- Routine Audits – Conduct inspections to ensure compliance with OSHA, CDC, and facility-specific infection control policies.
These steps collectively reduce exposure risks, protect staff and patients, and maintain a safe healthcare environment.
Partnering With a Certified Medical Waste Disposal Company
Partnering with the right medical waste disposal company is essential for maintaining safety, regulatory compliance, and operational efficiency.
- A reputable provider ensures that all waste, whether biohazardous materials, sharps, or PHI-containing items, is handled, transported, and destroyed according to OSHA, EPA, DOT, and HIPAA standards.
- They provide secure containers, properly trained personnel, and transparent documentation, including certificates of destruction, manifests, and chain-of-custody logs, giving healthcare facilities full accountability for their waste.
- Working with a certified vendor not only reduces the risk of regulatory violations but also saves time, lowers in-house handling costs, and ensures that your facility remains audit-ready at all times.
With over 25 years of experience serving Maryland, Virginia, and Washington, D.C., Secure Waste is a trusted partner for medical waste management. Fully licensed, bonded, and insured, we specialize in biohazardous waste, healthcare, and sharps disposal in Virginia, offering secure pickup, environmentally safe destruction, and complete compliance documentation. Our flexible schedules, no-contract policy, and transparent pricing make managing medical waste hassle-free and cost-effective. By choosing Secure Waste, healthcare facilities gain a reliable, professional partner that protects employees, patients, and the environment every step of the way.
Frequently Asked Questions
Are COVID-19 test kits considered regulated waste?
Yes, kits containing patient specimens or biohazard materials must be handled as infectious medical waste.
Can dental offices outsource their sharps and amalgam waste?
Absolutely; dental offices must use certified vendors for sharps, amalgam, and other regulated materials to ensure compliance with OSHA and EPA guidelines.
How should sharps be segregated from other medical waste?
Sharps must be placed immediately into labeled, puncture-resistant containers, kept separate from other waste to prevent injury and cross-contamination.
What labeling is required for medical waste containers?
Containers must be red or biohazard-labeled, leakproof, and puncture-resistant to indicate risk and ensure regulatory compliance clearly.
Do all healthcare workers need BBP training?
Yes, any staff potentially exposed to blood or other potentially infectious materials must receive BBP training before assuming job duties and annually thereafter.
What information is required on a medical waste manifest?
Include generator and transporter info, waste type and quantity, treatment facility, disposal method, and dates to ensure full traceability from generation to destruction.

Expert Medical Waste Management: With over 25 years of industry experience, Secure Waste is a trusted local leader in hazardous and biohazardous waste disposal across Maryland, Virginia, and Washington, D.C. Specializing in medical waste management, sharps needle disposal, and biohazard waste removal, the company ensures full compliance with federal, state, and local regulations while prioritizing environmental sustainability.
The company also offers additional services, including secure document shredding and sharps container sales, providing comprehensive solutions for healthcare facilities and businesses. Our cost-effective services help clients maintain regulatory compliance without unexpected costs.
With a commitment to customer satisfaction, Secure Waste offers tailored waste management plans that align with industry best practices. Their team of experts provides reliable, timely, and compliant services, making them the preferred choice for medical waste disposal. For a free waste quote or more information, visit www.securewaste.net






