Preventing Bloodborne Pathogens Exposure In Healthcare Setting – Expert Solutions For Healthcare Safety
Secure Waste explains exposure to bloodborne pathogens remains one of the most serious occupational hazards in healthcare environments. Workers routinely face risks associated with contact with blood and other potentially biohazardous infectious materials while performing essential patient care tasks. Without consistent safeguards, these exposures can lead to serious illness, long-term health consequences, and emotional stress for affected employees. Preventing exposure requires a structured, proactive approach that combines training, engineering controls, hygiene practices, and compliant biohazard waste management.
Bloodborne pathogens include a range of viruses and bacteria capable of causing infection when they enter the body through cuts, puncture wounds, or mucous membranes. While human immunodeficiency virus and hepatitis viruses are among the most widely recognized, many other pathogens pose risks in clinical environments. The most common source of exposure is percutaneous injury caused by contaminated sharps such as needles, lancets, scalpels, or broken glass. Exposure can also occur when blood or other infectious materials come into contact with the eyes, nose, mouth, or non-intact skin.
Understanding How Exposure Occurs
Healthcare workers encounter bloodborne pathogens during routine procedures such as injections, blood draws, wound care, and surgical interventions. Improper handling of biohazardous waste or disposal of sharps increases the likelihood of accidental injury. Exposure risks also arise when workers handle contaminated materials without adequate protection or when protective equipment is used incorrectly.
Other potentially infectious materials (OPIM) include certain body fluids and tissues that may be contaminated with blood. When these materials come into contact with mucous membranes or broken skin, the risk of infection increases. Understanding these exposure pathways is critical for implementing effective prevention strategies.
OSHA’s Role in Reducing Bloodborne Pathogen Risk
Secure Waste shares OSHA established the Bloodborne Pathogens Standard to protect workers who may reasonably be expected to come into contact with blood or other infectious materials as part of their job duties. This standard requires employers to implement safeguards that reduce exposure risk and to provide post-exposure evaluation and follow-up when incidents occur.
Compliance with OSHA requirements helps healthcare organizations move from reactive responses to proactive prevention. By identifying risks, training staff, and implementing controls, employers create safer working environments and reduce the likelihood of exposure incidents.
Hand Hygiene as a First Line of Defense
Proper hand hygiene is one of the most effective methods for preventing the spread of bloodborne pathogens. Healthcare workers must clean their hands immediately after contact with blood or infectious materials and after removing gloves or other protective equipment. Effective hand hygiene reduces the transfer of contaminants and protects both workers and patients.
Healthcare organizations should ensure that handwashing stations are readily accessible in areas where patient care occurs. Staff must be trained on proper handwashing techniques and encouraged to use these facilities consistently. Readily available supplies and clear expectations reinforce safe behavior.
Safe Sharps Disposal Practices
Sharps disposal plays a critical role in preventing bloodborne pathogen exposure. Used needles and other sharp instruments must be placed immediately into puncture-resistant containers designed specifically for sharps (Sharps Containers). These containers reduce the risk of accidental injury by preventing overfilling, leakage, or protrusion of sharp objects.
Sharps containers should be placed as close as possible to the point of use so that workers can dispose of items safely without transporting them through patient care areas. Proper placement and routine monitoring of container fill levels are essential to maintaining a safe environment.
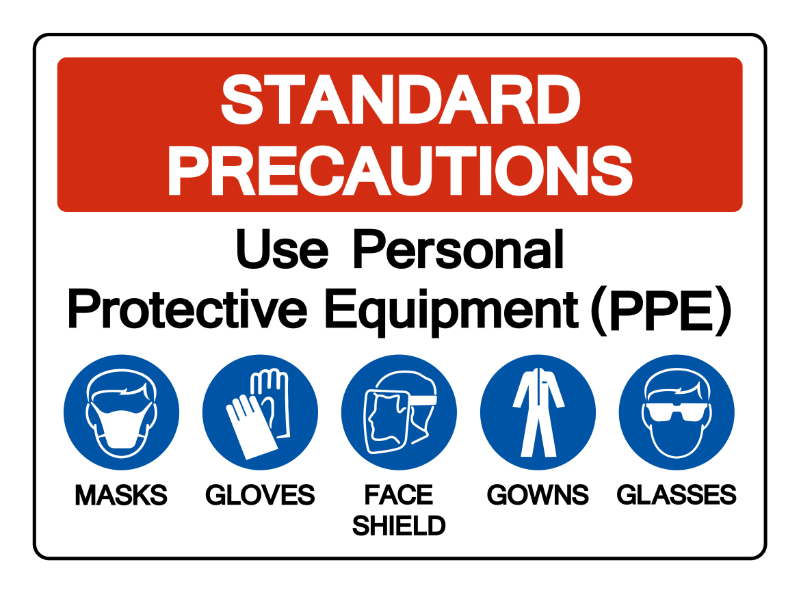
Proper Use and Disposal of Personal Protective Equipment
Personal protective equipment acts as a barrier between workers and potentially infectious materials. Gloves, gowns, masks, and eye protection must be readily available and properly fitted for all affected employees. Workers should be trained on when and how to use protective equipment correctly.
Equally important is the proper removal and disposal of used protective equipment. Contaminated PPE must be discarded in designated containers to prevent secondary exposure. Clear procedures and designated disposal areas help ensure consistent compliance.
Comprehensive Training and Ongoing Education
Training is a cornerstone of bloodborne pathogen prevention. Employees who face potential exposure must receive detailed orientation and regular refresher training that covers exposure risks, preventive measures, and response procedures. Training should reflect real-world scenarios and be updated whenever job duties or procedures change.
Accessible training options, including digital learning platforms, allow staff to complete required education efficiently while ensuring documentation is maintained. Ongoing education reinforces awareness and helps workers remain vigilant about safety practices.
Bloodborne Pathogen Risks Beyond Hospitals
While hospitals often receive the most attention, bloodborne pathogen risks exist across many healthcare and service environments. Dental practices, outpatient clinics, laboratories, long-term care facilities, and emergency response settings all face exposure risks due to the presence of sharps and bodily fluids.
Organizations in these settings must implement exposure control plans that outline vaccination availability, post-exposure protocols, and waste handling procedures. Consistent application of safety standards across all environments reduces risk for workers and the public.
The Importance of Proper Waste Management
Safe handling and disposal of contaminated waste is essential to preventing exposure incidents. Improper disposal of sharps and regulated waste increases risk for healthcare workers, custodial staff, and waste handlers. Partnering with an experienced waste management provider ensures that waste is handled, transported, and processed in accordance with safety and regulatory standards.
Secure Waste supports healthcare organizations by providing compliant sharps and medical waste solutions designed to reduce exposure risk and support OSHA-aligned safety practices. Proper waste management strengthens infection prevention efforts and contributes to safer workplaces. Learn more at https://www.securewaste.net/.
Building a Culture of Prevention
Preventing bloodborne pathogen exposure requires more than compliance with regulations. It requires a workplace culture where safety is prioritized, concerns are addressed promptly, and employees feel empowered to follow best practices. Leadership commitment, consistent training, and reliable systems work together to create safer environments.
When safety measures are embedded into daily operations, exposure incidents become less frequent and less severe. This proactive approach protects workers, improves morale, and supports long-term organizational resilience.
Final Takeaway
Bloodborne pathogen exposure remains a significant occupational risk in healthcare and related environments. By understanding exposure pathways, implementing OSHA-aligned safeguards, promoting hand hygiene, ensuring proper sharps disposal, and partnering with responsible waste management providers, organizations can significantly reduce risk. Preventing exposure protects workers, patients, and communities while supporting a safer, more compliant healthcare system.

Expert Medical Waste Management: With over 25 years of industry experience, Secure Waste is a trusted local leader in hazardous and biohazardous waste disposal across Maryland, Virginia, and Washington, D.C. Specializing in medical waste management, sharps needle disposal, and biohazard waste removal, the company ensures full compliance with federal, state, and local regulations while prioritizing environmental sustainability.
The company also offers additional services, including secure document shredding and sharps container sales, providing comprehensive solutions for healthcare facilities and businesses. Our cost-effective services help clients maintain regulatory compliance without unexpected costs.
With a commitment to customer satisfaction, Secure Waste offers tailored waste management plans that align with industry best practices. Their team of experts provides reliable, timely, and compliant services, making them the preferred choice for medical waste disposal. For a free waste quote or more information, visit www.securewaste.net